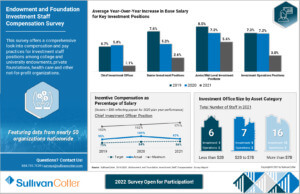
INFOGRAPHIC | Endowment and Foundation Investment Staff Compensation Survey
The world of philanthropy continues to thrive as foundations and endowments identify new giving opportunities and develop innovative programs and services to support them.
This requires a highly unique and specialized workforce, however, and organizations are seeking guidance on how to develop and elevate their talent management and investment strategies.
With unique insight into base salary, total cash compensation, incentive plan design and more, SullivanCotter's Endowment and Foundation Investment Staff Compensation Survey can serve as an important resource for organizations looking to benchmark key investment staff positions including chief investment officer, managing director, director, manager, analysts, and operations staff.
View highlights from the 2021 survey results to learn more!
DOWNLOAD INFOGRAPHIC
2022 Physician Fee Schedule: Understanding Changes to Split/Shared Visits
Download Full Article
Each year, the Centers for Medicare and Medicaid Services (CMS) incorporates changes in policy, regulations and requirements for billing under the Medicare Physician Fee Schedule (PFS). These changes are often adopted by commercial payers.
On November 2, 2021, CMS released the final rule for the 2022 PFS that included changes to split/shared visits scheduled to go into effect on January 1, 2022. The proposed changes included some important considerations related to the conditions for submitting split/shared visits for reimbursement and have the potential to alter the existing workflow of physicians and advanced practice providers (APPs) related to billing for split/shared encounters.
While some changes took effect in 2022, a number of the most impactful changes to split/shared billing were delayed to January 1, 2024. The 2023 PFS final rule indicates CMS’ desire to make significant changes to split/shared visits while allowing organizations time to prepare.
Split/Shared Visits
According to the Medicare Claims Processing Manual Publication #100-04:
“A split/shared E/M visit is defined by Medicare Part B payment policy as a medically necessary encounter with a patient where the physician and a qualified non-physician provider each personally perform a substantive portion of an evaluation and management (E/M) visit face-to-face with the same patient on the same date of service. A substantive portion of an E/M visit involves all or some portion of the history, exam or medical decision-making key components of an E/M service. The physician and the qualified NPP must be in the same group practice or be employed by the same employer.”
Split/shared E/M visits are only applicable in the hospital inpatient and hospital outpatient departments using provider-based billing and emergency room sites of service for all professional encounters currently except for critical care services, procedures, or time-based codes (e.g., prolonged service time).
What is Changing?
The 2022 final rule included several changes that are designed to reflect current clinical practice, recognize APPs’ evolving role as members of the care team, reduce duplication of services and clarify the conditions of payment for these types of services.1,2 These changes were implemented beginning in 2022 with additional changes identified for implementation in 2024. The most significant change is moving the split/shared visit from an E/M and medical decision-making based attribution to a time-based attribution. Under the current medical decision-making rubric, split/shared visits are typically billed by physicians, assuming specific conditions of collaboration have been met (e.g., face to face encounter, contributing to the evaluation, management or medical decision, employed by the same group or employer). In 2022, changes include the allowance of time-based accounting for a split/shared visit where “the practitioner who provides the substantive portion of the visit (more than ½ of the total time spent) would bill for the visit.” In 2022 and 2023, split/shared visits can be submitted using the current medical decision-making methodology or the new time-based methodology. Other changes applicable in 2022 include the ability for critical care services to be reported as split/shared, and the requirement that a new billing modifier be added for all shared visits. A survey performed by SullivanCotter of National APP Advisory Council (NAAC) members found that 54% of organizations were still using split shared billing.3
The greatest impact on split/shared visit billing is set to occur in 2024 when all shared visits must be billed using the time-based methodology where the practitioner who provides the substantive portion of the visit (“more than ½ of the total time spent”) bills for the visit1. In 2022 and 2023, the impact of the split/shared change will likely be modest but will allow organizations time to better understand the degree of split/shared billing that occurs within their organizations through the shared visit modifier requirement.
In 2024, the impact on attributed wRVUs for physicians and APPs providing services in the inpatient setting could be significant. The time-based methodology will require physicians to have greater than 50% of the time spent with a patient in order to bill and receive wRVU attribution. Because of this change, in 2024, the same patient volume using current split/shared workflows could result in an increase in reported APP wRVUs and a corresponding decrease in reported physician wRVUs. This change could also result in an overall decrease in professional collections (to account for the 15% difference in Medicare physician and APP reimbursement levels for the same service).
When accounting for time, CMS identified these specific activities:2
- Preparing to see the patient (for example, review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record (Note: CMS has stated it may be helpful for each individual to document their own participation in the medical record in order to determine the substantive time).
- Independently interpreting results (not separately reported).
- Communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
Example
A hospitalized patient with a diagnosis of pneumonia is being cared for by the hospital medicine team composed of a physician and an APP. On hospital day 2, the APP sees the patient in the morning and spends 25 minutes with the patient performing a focused history and physical, reviewing the morning labs and providing patient education related to the course of treatment with the patient and their family. Based on a detected decrease in lung sounds during the lung exam, the APP orders a chest x-ray. Later in the day, the physician and the APP spend an additional 10 minutes together to make afternoon rounds and review the chest x-ray findings, make changes in treatment, and meet with the patient to review the chest x-ray results (35 minutes in total for the APP and 10 minutes total for the physician).
The hospital medicine team bills the encounter as 99233 (subsequent hospital care level 3). Under the historical medical decision-making approach, this could be billed by the physician as a split/shared visit (assuming all of the other criteria were met) or by the APP (paid at 85% of the allowed amount for Medicare patients).
Under the time-based billing approach, the visit could only be billed by the APP as the APP provided the majority of the encounter (35 out of 45 minutes or 78% of the total time spent in the encounter). As the physician would not receive wRVU or reimbursement credit for this visit using this methodology, this could impact credited physician productivity and, for organizations using productivity-based compensation models, both physician and APP compensation.
What Now?
Current care delivery models should be reevaluated when developing a strategy to transition to time-based billing for split/shared visits. It is important to design an effective and transparent workflow that allows for top-of-licensure operation and minimizes any competition for credit. With changes imminent, organizations can take the following steps to prepare:
- Assess the current state of split/shared billing at your organization.
- Evaluate current care team composition and work responsibilities to determine the optimal team composition and anticipated wRVU attribution impact to ensure that providers are efficient and optimally utilized.
- Assess the impact on specific patient workflows (e.g., new patients, established patients, discharges) where split/shared visits are utilized today.
- Identify types of encounters that could be performed solo by the APP thus allowing physician to see other patients.
- Consider if modifications to physician and APP compensation arrangements are needed to ensure financial sustainability and regulatory compliance. Be aware these changes may influence the reported wRVU and compensation per wRVU 2023 survey report data.
Sources
1. Calendar Year (CY) 2022 Medicare Physician Fee Schedule Final Rule. Published November 2, 2021. Retrieved from https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-final-rule
2. RIN 0938-AU42 Medicare Program; CY 2022 Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment Policies. Published November 19, 2021. Retrieved from https://www.federalregister.gov/d/2021-23972
3. National APP Advisory Council - Fall 2022 Pulse Survey
PRESS RELEASE | Enhanced Benchmarking Capabilities Added to SullivanCotter’s Provider Performance Management Technology™
Enhanced Benchmarking Capabilities Added to SullivanCotter’s PPMT™
Chicago, IL | October 19, 2021 11:00 AM Eastern Daylight Time
SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, announces significant benchmarking enhancements to its growing Provider Performance Management TechnologyTM (PPMT™) platform. PPMT is an industry-first, cloud-based product that engages clinicians and informs leaders through transparent performance-based compensation administration, contract management, and analytical and reporting capabilities.
PPMT’s fall product release includes new configurability options for its already powerful benchmarking capabilities, including the ability to select months for productivity benchmarks and identify and benchmark physicians who specialize in multiple service areas. “Our latest enhancement allows users to remove abnormally low productivity months, particularly like we’ve seen with COVID-19, to make the data set more relevant. This can also be beneficial when clinicians take a leave of absence and more,” said Shelly Slowiak, Director, Product Support, PPMT, SullivanCotter.
PPMT’s current functionality enables clients to view both individual and collective physician performance relative to their own custom organizational benchmarks. This allows physicians and leaders to monitor real-time productivity and compare to the organization’s key compensation productivity thresholds. In addition to displaying wRVU productivity, users may compare total cash compensation (TCC) and metrics to external and internal benchmarks for both full-time and split clinical roles.
Designed to address a spectrum of physician, leadership and other key stakeholder needs, PPMT combines years of healthcare compensation insight and expertise with an intuitive and automated technology platform to help drive provider performance and support the transition from volume- to value-based care.
“Based on the evolving needs of our clients, SullivanCotter continues to invest in and improve our technology products. Alongside Benchmarks360™, which enables clients to analyze and visualize compensation, clinical productivity, and workforce perceptions, we continue to offer our clients additional ways to benchmark pay and productivity,” said David Schwietz, Chief Information Officer, SullivanCotter.
For more information on these enhancements or our entire suite of Provider Performance Management Technology™, visit www.sullivancotter.com/PPMT or contact us at 888.739.7039.
About SullivanCotter
SullivanCotter partners with health care and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology products to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON NEWSDIRECT
ARTICLE | Key Agenda Items for Board Committees
Featured in McDermott Will & Emery's newly published e-book from its Governing Health series
SullivanCotter’s Kathy Hastings, Executive Workforce Practice Leader, and Tim Cotter, Managing Director, have contributed two chapters to a newly published e-book from McDermott Will & Emery entitled, Key Agenda Items for Board Committees: A Briefing for Governance and Executive Leadership.
Their two chapters include:
- 10 Focus Areas for Your Human Capital Committee
- Top 10 Diligence Questions for Executive Compensation Committees
Access the E-Book Here
PRESS RELEASE | SullivanCotter's 2021 Physician and APP Compensation and Benchmarks
SullivanCotter Announces the Release of 2021 Physician and Advanced Practice Provider Compensation and Productivity Benchmarks
Chicago, IL | August 24, 2021 02:42 PM Central Daylight Time
SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, is excited to announce the release of its 2021 compensation and productivity benchmarks for nearly 260,000 physicians, physician leaders and advanced practice providers nationwide.
Organizations are currently struggling to understand how to utilize the new survey benchmarks and effectively adjust for a number of unprecedented changes from last year and, as a result, are looking for more reliable and stable datasets moving forward.
“This year more than ever, hospitals and health systems require critical data-driven insights as they look to normalize the impact of COVID-19 on clinical workforce compensation and productivity and address substantial modifications to the 2021 Physician Fee Schedule. To help clients plan for 2021 and beyond, SullivanCotter will be offering enhanced analyses and reporting as well as guidance on best practices for evaluating the newly released survey data,” said Chris Brandt, Senior Director, Data Analytics and Reporting, SullivanCotter.
In addition to standard, non-adjusted benchmarks as historically reported, organizations who purchase an eligible survey report will receive complimentary COVID-19-adjusted work RVU and TCC per work RVU data – providing greater insight into the effect of the pandemic and enabling hospitals, health systems and medical groups to quickly measure the impact on compensation and productivity within their organizations.
Newly available for purchase this year are three tiers of detailed productivity reporting – including monthly work RVU volumes by specialty in addition to individual CPT code-level details. When combined with SullivanCotter’s innovative Benchmarks360™ platform, organizations can more effectively analyze and visualize this data with access to dynamic filters, multi-year coding profiles, and annual updates to CPT codes.
SullivanCotter will also be offering adjusted benchmarks for total cash compensation, work RVUs, collections and other related ratios for use in conjunction with the 2021 Physician Fee Schedule. This includes proprietary data from SullivanCotter's 2021 surveys as well as other third-party market datasets (with appropriate licensing and non-disclosure agreements in place).
The 2021 surveys are now available for purchase at SullivanCotter.com. To learn more about this year’s enhanced reporting and analyses, please contact surveys@sullivancotter.com or dial 888.739.7039.
About SullivanCotter
SullivanCotter partners with health care and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology products to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON NEWSDIRECT
PRESS RELEASE | Reid Health Selects SullivanCotter’s Provider Performance Management Technology™
Reid Health Selects SullivanCotter’s Provider Performance Management Technology™ to Provide Transparency and Insight into Physician Pay and Performance
Chicago, IL | September 14, 2021 07:00 AM Central Daylight Time
SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, has partnered with Reid Health to implement its comprehensive Provider Performance Management Technology™ (PPMT™).
Reid Health is a nationally recognized regional referral center in Richmond, Indiana, with a 200+ bed hospital and physicians network meeting health care needs in east central Indiana and west central Ohio. By leveraging PPMT™, an industry-first, cloud-based product that enables physician and advanced practice provider (APP) engagement through transparent performance-based compensation administration and analytical capabilities, the organization proactively enables physicians to review their productivity and compensation calculation details with insights into patients, visits, and performance. “With PPMT’s powerful heat map, we are able to drill down into our providers’ productivity and identify those with potential capacity. This helps us uncover community outreach opportunities, enabling providers to increase patient access and boost productivity,” said Amy Gowin, Director of Finance, Reid Health Physician Associates.
Along with providing increased transparency, PPMT™ has reduced compensation planning and administrative challenges by automating Reid Health’s complex provider compensation contract calculations and notifications. With PPMT™, budgeted wRVUs are loaded into the system for use in compensation calculations and forecasting for the upcoming fiscal year. “PPMT™ provides Reid Health’s physicians, like myself, a transparent view of my clinical work performance and how I will be compensated for it. It provides timely, accurate, and actionable data, and I appreciate the ability to see my data promptly,” said Dr. Rohit Bawa, Chair, Network Operations Council, Reid Health Physician Associates. “Additionally, as a physician leader, the software enables clinician engagement through transparency of their performance”.
“We are excited about the operational efficiencies and physician trust and engagement gained by our clients. PPMT™ provides physicians, administration, and leadership with a single source of reliable compensation and performance information. We are thrilled to partner with Reid Health,” said Shelly Slowiak, Director, Product Support, PPMT™, SullivanCotter.
PPMT™ includes four dynamic modules, including Provider Performance Management, Provider Productivity Insights, Compensation Management Analytics, and Contract Lifecycle Management, powered by Ntracts. Reid Health plans to use all modules to help support its growing network of providers, allowing for a more cohesive approach to compensation and performance management.
For more information on Provider Performance Management Technology™, visit www.sullivancotter.com/PPMT or contact us at 888.739.7039.
About SullivanCotter
SullivanCotter partners with healthcare and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology products to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON NEWSDIRECT
The Governance Institute | Executive Compensation and Governance Trends for 2021 and Beyond
READ FULL ARTICLE
As the response to COVID-19 continues, healthcare organizations nationwide face an uncertain environment in the near-term as vaccination rates slow, virus variants appear, and operational recovery from the pandemic accelerates. Additionally, there are a myriad of intermediate and longer-term forces at play—such as reimbursement pressures, technology disruption, workforce burnout and labor shortages, new competitive threats, and regulatory changes—that require attention.
The complexity of healthcare organizations continues to increase as pressures mount for financial sustainability, diversification, efficiency, and new care delivery models. Leadership retirements and burnout brought on by the pandemic have exacerbated the limited supply of executive talent with the skills, experience, and competencies needed to lead these complex organizations through significant change. As healthcare organizations and their boards confront this environment, executive compensation programs, talent strategies, and governance will continue to adapt.
In this article, we recap the response of healthcare organizations in 2020 and outline priorities for 2021 and beyond.
Pandemic Response: Impact on Executive Compensation
Compensation committees and healthcare leaders took several actions during 2020 in response to the pandemic:
- Prioritizing the broader workforce: The healthcare workforce rose to the challenge of meeting community needs as the pandemic took hold. The workforce made extraordinary professional and personal sacrifices to ensure patient needs were met. There was a focus on ensuring the broader workforce was supported through the implementation of special incentives and pay differentials, accommodations for childcare and other personal needs, and the delivery of base salary increases when financially viable (with budgets in the 2 to 3 percent range).
- Lowering base salary budgets: Executive salaries were impacted with many freezing, temporarily reducing, or moderating increases. Broad-based workforce increases were prioritized over consideration of executive increases. About one-third of healthcare executives did not receive a base salary increase between 2020 and 2021. Overall, the median base salary increase for healthcare executives was 2 percent, which was lower than the initially projected prepandemic 2020 salary increase budget of 3 percent.
- Changing incentives to reflect the COVID-19 response: Executive incentive plans changed. Performance measures and goals were adjusted by many organizations to reflect shifting priorities in response to COVID-19. The adjudication of incentives was holistic as business judgment was applied to consider performance, pandemic response, treatment of the workforce, and stakeholder perspectives. Approximately 15 percent of executives did not receive an annual incentive award. For those who did receive an award, the typical payout as a percentage of the target opportunity was lower than in prior years.
- Rewarding positions leading COVID-19 response and transformation: Higherthan-average salary increases were observed for a number of positions that led the COVID-19 response or longer-term transformation efforts (e.g., Chief Operating Officer, Chief Medical Officer, Chief Technology Officer, Chief Nursing Officer, and Top Facilities Executive). In addition, more organizations reported emerging leadership positions in key functions, including telehealth, ambulatory care, digital strategy, and diversity, equity, and inclusion.
Key Priorities for 2021 and Beyond
There are five priorities for compensation committees as pay determinations are made this year and the executive compensation program’s effectiveness is considered.
- Compensation actions: Plan for flexibility as 2021 compensation decisions are made, to recognize the ongoing impact of the pandemic on operations:
-
- Executive base salary increase budgets are projected to rebound to prepandemic norms of 3 percent, although some organizations may provide more significant increase budgets to respond to retention and competitiveness needs.
- Additional salary adjustments are anticipated for select roles based on data from SullivanCotter’s 2021 Health Care Management and Executive Compensation Survey (e.g., physician leaders and executives in operations, technology, nursing, supply chain, and quality).
- Business judgment may be needed when determining incentive awards for 2021 performance, to account for the unanticipated effect on performance goals and priorities, as well as competitiveness considerations and stakeholder optics.
-
- Compensation philosophy: Ensure the executive compensation philosophy supports the organization’s recruitment, retention, and motivation needs:
-
- Peer groups that reflect the potential for recruiting talent from outside of traditional healthcare peers, including broader industry peers.
- Flexibility so that compensation can be appropriately competitive rather than tied to a specific percentile, to allow for variation based on a role’s organization impact, performance, and other factors.
- Allowance for variation in pay models for different business units (e.g., health plans, long-term care, and business ventures).
-
- Performance and incentives: Examine the executive incentive plan to ensure it aligns with new performance priorities and measures of success:
-
- Measures and goals that capture operating and strategic objectives, such as financial sustainability, patient experience, community benefit, care access, and deployment of new delivery models (e.g., telehealth).
- The degree of stretch in performance goals to help ensure meaningful performance is attained for corresponding payouts.
- Consider long-term incentives that reward for attaining multi-year transformation objectives.
- Consider the impact of regulatory developments on incentives (e.g., actions to encourage more competition).
-
- Executive talent strategy and succession: New skills and competencies will be required to achieve organizational goals. Plus, organizations should plan for executive turnover due to the competitive talent market and career/retirement changes accelerated by the pandemic:
-
- Expect to recruit from expanded talent markets (including for-profits) for select positions based on specific organizational needs (e.g., telehealth/digital executives from IT and population health executives from managed care organizations).
- Anticipate the need to provide highly competitive pay for new recruits.
- Refine executive succession plans (including the identification of emergency successors) based on the organization’s talent needs.
- Ensure there is a strong talent pipeline and determine if talent will be developed internally or recruited externally.
- Assess organizational structure and spans of control to support the delivery of cost-effective and quality care using new operating models.
- Monitor the impact of regulatory developments (e.g., potential restrictions on non-competes).
-
- Diversity, equity, and inclusion: Determine how diversity, equity, and inclusion (DE&I) priorities will impact the executive talent strategy, recruitment/retention, program design, and governance:
-
- Assess executive and broader workforce diversity through the use of governance dashboards and other committee reporting; understand how talent strategies and succession plans are considering DE&I.
- Ensure that pay equity is assessed and that processes and policies are in place to monitor and maintain pay equity over time.
- Consider the use of DE&I measures in annual and/or long-term incentive programs.
- Expect highly competitive compensation for DE&I leadership roles.
-
➜ Key Considerations for Compensation Committees
As healthcare organizations and their boards address changing performance priorities and leadership recruitment and retention needs during this uncertain time, executive compensation programs, talent strategies, and governance will continue to adapt. Compensation committees should expect an active agenda in this environment, focusing on five priorities:
-
- Ensuring compensation actions (base salary increase budgets, market adjustments, and incentives for 2021 performance) account for the rebound in the industry, the highly competitive talent market, and the challenges of operating in the environment. Anticipate the use of business judgment as actions are determined.
- Align the compensation philosophy to evolving needs and provide for the flexibility to recruit, retain, and reward talent in line with changing needs.
- Adjust the incentive compensation program to ensure performance measures reflect evolving priorities and payouts align with meaningful performance outcomes.
- Review executive talent strategies and succession plans to account for new skill requirements and expected emergency and long-term succession requirements.
- Incorporate diversity, equity, and inclusion (DE&I) into the compensation strategy—review pay equity, consider the role of the compensation committee in DE&I governance, and determine how the incentives and other programs can further DE&I goals.
Conclusion
Healthcare organizations increasingly are focused on opportunities emerging from the pandemic. Compensation committees should expect continued refinements to the executive compensation program and talent strategies to support organization and performance needs.
The Governance Institute thanks Bruce Greenblatt, Managing Principal, SullivanCotter, Inc., for contributing this article. He can be reached at brucegreenblatt@sullivancotter.com.
Featured in the September edition of The Governance Institute’s E-Briefings, SullivanCotter recaps the response of healthcare organizations in 2020 and outlines priorities for 2021 and beyond.
Reprinted with permission from The Governance Institute, San Diego, CA, (2021), (Bruce Greenblatt, SullivanCotter. Executive Compensation and Governance Trends for 2021 and Beyond).
READ FULL ARTICLE
INFOGRAPHIC | Optimizing Utilization of the Advanced Practice Provider Workforce
The focus on team-based care will require healthcare organizations to optimize the performance of all members of the care team.
Many hospitals and health systems continue to grow their advanced practice provider (APP) workforce as they realize important operational benefits such as improving the quality of care, increasing patient access, enhancing provider satisfaction and reducing costs.
However, this growth is often organic and can result in significant variation in APP utilization and organizations must develop strategic models of care in order to effectively integrate, optimize and engage this growing workforce.
DOWNLOAD INFOGRAPHIC
Case Study | Optimizing Utilization of the Advanced Practice Provider Workforce
The focus on team-based care will require healthcare organizations to optimize the performance of all members of the care team.
Learn more about how a leading academic medical center assessed opportunities for care team optimization and redesigned their APP workforce.
View Case Study
How to Take Advantage of New Stark Law Compliance Regulations
Now that the government has allowed for some regulatory relaxation, how can healthcare providers take advantage while still mitigating risk?
SullivanCotter's Ron Vance, Managing Principal, recently joined a panel of experts to discuss changes to the Stark Law and how organizations can position themselves to best ensure compliance.
Listen to the webinar recording or download the discussion highlights to gain a better understanding of the regulatory updates and how they impact provider arrangements, as well as how healthcare providers can and should be proactive in reconciling the management of those arrangements and the data surrounding them to mitigate potential risk and exposure.
Modern Healthcare | 2021: Annual Executive Compensation Article
Healthcare organizations focus on recruitment and retention of key executive talent as industry attention on diversity, wellness and other long-term transformations intensifies.
As the healthcare industry continues to respond to the extraordinary and unprecedented impact of the COVID-19 pandemic, organizations are evaluating and adjusting their executive compensation practices to adapt to the changing landscape.
Competition to fill executive positions is becoming increasingly challenging with limited talent available with the skills, experience and competencies needed to successfully lead complex healthcare organizations through the post-pandemic environment. In addition, the definition of organizational success is changing as strategic and operating plans are updated.
Featured in Modern Healthcare’s annual executive compensation article, SullivanCotter’s Bruce Greenblatt and Tom Pavlik share data from SullivanCotter’s 2021 Health Care Management and Executive Compensation Survey, and highlight some of the actions organizations are taking to draw in and retain executive talent, while also focusing on the recovery that lies ahead during such an uncertain time.
READ FULL ARTICLE
APPs: 2021 Evaluation and Management CPT Codes
Part II: Understanding the Impact on Advanced Practice Providers
DOWNLOAD FULL ARTICLE
RELATED CONTENT:
PART I | 2021 E&M CPT Code Changes: Understanding the Impact on Physician Compensation
INFOGRAPHIC | Considerations for Addressing the 2021 E&M Work RVU Changes
ARTICLE | Navigating Change: Implications of the 2021 Physician Fee Schedule
SullivanCotter's CPT Advisory Services and Technology Solutions
BACKGROUND
Every year, the Centers for Medicare and Medicaid Services (CMS) evaluates the recommendations of the American Medical Association’s Relative Value System Update Committee and conducts its own review of the Work Relative Value Unit (wRVU) values associated with each Current Procedural Terminology (CPT) code to determine if revisions are needed based on the time, skill, training and intensity necessary to perform each service. The degree of change varies from year to year, and the impact on individual specialties depends on which codes are modified and the extent to which the codes are adjusted.
CURRENT SITUATION
At the end of 2019, CMS proposed widespread modifications to a subset of the Evaluation and Management (E&M) CPT codes (99201-99215) that include face-to-face office visits and other outpatient services for new or established patients. The goal of the adjustments is to provide an increase in certain wRVU values to address added responsibilities clinicians have absorbed over the last five years, reduce documentation requirements, recognize extended patient visits, and account for qualified, severe or complex chronic conditions. On December 1, 2020, CMS finalized the 2021 Physician Fee Schedule – which went into effect on January 1, 2021.
Additionally, in response to COVID-19, CMS has implemented new guidance as it relates to telehealth services. Although it is unknown whether these CPT code changes will be maintained or altered as the pandemic subsides, the agency has indicated a desire to make longstanding revisions to telehealth visit valuations. While the 2021 Physician Fee Schedule final rule permanently expanded some of the telehealth changes for rural communities, the adoption of the telehealth changes has not been identified as permanent.
In Part I of this series, SullivanCotter explored the impact of the E&M code changes on physician compensation and productivity levels as well as other implications health care organizations must be mindful of as they plan physician compensation for 2021 and beyond. For additional background, Part I also included a detailed summary of the final changes – including greater insight into the “Patients Over Paperwork” goal, the results of a work-effort/time-study commissioned by CMS, and two related add-on codes.
As we continue to assess how these changes affect the clinical workforce, Part II in this series reviews the impact on advanced practice providers (APPs).
ADDRESSING THE IMPACT ON ADVANCED PRACTICE PROVIDERS
Based on the overlapping scope of services performed by APPs and physicians, CMS modifications to CPT code valuations will impact both APPs and physicians. At a broad level, these changes include:
- An increase in wRVUs for most office-visit E&M CPT codes due to added responsibilities clinicians have absorbed over the last five years.
- A 3.3% reduction in the Medicare conversion factor (now $34.89) for physician fee schedule payments to maintain budget neutrality that impacts all E&M services no matter who provided the service.
- An add-on code to recognize extended office-visit time.
Due to the differences in practice patterns between APPs and physicians, there will be some variation in how the changes will impact APPs as compared to physicians. The differences may include the following factors:
- APPs often perform a greater amount of non-billable work and provide services covered under a global visit.
- APPs may see lower acuity patients in some specialties or settings.
- In our analysis of reported CPT data, APPs in surgical specialties report E&M services (e.g. office visits) as a greater proportion of their overall work compared with physicians who report a relatively greater proportion of procedures and surgeries.
Additionally, there are some APP-specific provisions that may affect scope of practice:
- Effective as of January 1, 2021, Medicare now permits physician assistants (PAs) to perform diagnostic tests in accordance with supervisory requirements outlined in state law rather than in Medicare’s general supervision requirements. This change means that PAs are no longer subject to two sets of requirements as Medicare now defers to state policy instead. This helps to reduce administrative burden and potential confusion within organizations about which regulations to follow.1
- The rule for 2021 allows all APPs (APRNs and PAs) to supervise the performance of diagnostic tests in accordance with their state’s scope of practice. Previously, only physicians were authorized to do so. The ability of APPs to be able to perform diagnostic tests will likely have an impact on APP procedural specialties like interventional radiology and some medical specialties such as cardiology and gastroenterology.2
As healthcare organizations absorb these changes and plan for what lies ahead, there are a number of practical implications for APP productivity and compensation to keep in mind. This article helps organizations to understand and address the impact on APP productivity levels in various specialties, temporary changes to telehealth codes, and unintended consequences for APP productivity-based incentive plans. It also highlights other variables that could influence the assessment of APP productivity – such as survey benchmarks and how to utilize these going forward.
WORK RVU ADJUSTMENTS
The impact of the wRVU changes may result in material shifts in wRVU productivity for APPs. According to SullivanCotter’s 2020 Advanced Practice Provider Compensation and Pay Practices Survey, over 40% of APPs work in office-based specialties and ambulatory clinics.
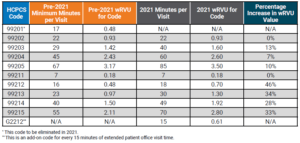
Table 1 below compares the pre-2021 E&M code time allocation and wRVUs to the January 2021 changes.
Note that the established office-visit codes 99212-99215, which are the most frequently used office-visit codes, show the most significant increases between 28%-46%. To balance CMS’ expenditures, the 2021 conversion factor, which is multiplied by total RVUs to determine Medicare payments to physicians and APPs, has dropped by 3.3% from $36.09 to $34.89. SullivanCotter notes that approximately half of the rate reduction mitigation is designated only for the 2021 calendar year as a result of the Consolidated Appropriations Act of 2021 – meaning an additional conversion factor reduction looms for 2022.
This change impacts all clinicians regardless of specialty and, combined with the E&M wRVU increases, creates a redistribution of federal payer reimbursement from proceduralists and hospital-based specialties to cognitive specialties.
Table 1: Time Allocations and wRVUs Adjustments: Current Versus 2021
Additionally, there are CPT code changes related to COVID-19 that will impact both physician and APP compensation and productivity. In March 2020, CMS expanded the Medicare telehealth coverage waiver to enable beneficiaries to receive a wider range of health care services from clinicians without having to travel to a health care facility. The announcement expanded previous telehealth coverage for beneficiaries living in rural areas who were able to receive care at a local facility with a clinician from a remote area.3
Under the new provisions, all beneficiaries are able to receive telehealth coverage. Effective March 2020, telehealth services were paid under the Medicare Physician Fee Schedule at the same rate as in-person services.
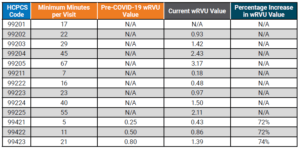
Table 2 below compares the pre-COVID-19 E&M code time allocation and wRVUs to the changes made in March 2020. It is unclear how long CMS plans to keep the expanded rates in place.
Table 2: Telehealth wRVU Adjustments: Results of 2020 Waivers
THREE IMPORTANT POTENTIAL IMPACTS TO APP PRODUCTIVITY LEVELS AND RESULTING COMPENSATION AND BENCHMARK MEASUREMENTS
1. How will the 2021 wRVU changes impact the measurement of APP productivity?
This common question is complex for APPs given that productivity benchmarks have generally been difficult to collect and interpret due to the wide variation in how APPs are utilized – even within the same specialty. Historically, productivity data has been absent, inconsistent or inaccessible due to the variety of billing practices used to capture APP work effort including shared visits and incident-to billing. Additionally, APPs often perform more non-revenue generating work compared to physicians in the same specialty (e.g., global visits) – contributing to inconsistency and difficulty in collecting the data.
To help analyze the impact, SullivanCotter used its proprietary database consisting of individual CPT code volumes and modifiers for approximately 3,000 APPs across 45 different specialties. Two sets of wRVU productivity benchmarks were calculated for comparison. One is based on the pre-2021 wRVU values, and one is based on the 2021 wRVU values. By keeping volumes and distribution consistent, the resulting change in wRVU productivity is due entirely to the E&M wRVU adjustments.
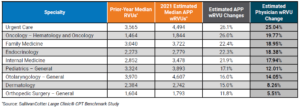
Summary findings indicate that of the 45 specialties reviewed, the average change for all specialties due to the E&M adjustments is 14.6%. As shown in Table 3 below, nearly half (44.4%) of wRVU benchmarks increased between 6% and 17%. An additional 44.4% of specialties were impacted by changes greater than 17%. Only two specialties had changes of less than 1%.
Table 3: Overall APP Specialty Impact of 2021 E&M Changes
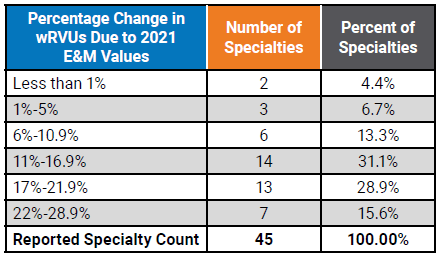
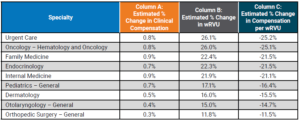
Table 4 below shows a representative sample of the resulting impact at the specialty level. This represents a significant change to wRVU benchmarks in many specialties and will be important for organizations to understand the implications to APP compensation payouts and affordability in all of the various specialties and care teams. Comparing the estimated wRVU changes for APPs and physicians in the same specialty shows general alignment in the medical and primary care specialties with a greater impact on the APPs in surgical specialties due to the higher utilization of E&M visits by APPs compared to physicians.4
Table 4: Median wRVU Impact of 2021 E&M wRVU Changes
2. How will wRVU changes impact compensation for APPs differently than physicians?
The impact will vary for a few notable reasons.
According to SullivanCotter’s 2020 Advanced Practice Provider Compensation and Pay Practices Survey, only 56% of organizations use wRVU data to adjust APP compensation as compared to greater than 90% for physicians.5,6 Because APP compensation is typically salary-based, APPs are less susceptible to compensation impacts due to the CPT adjustments.
Additionally, nearly half of APPs with an incentive component in their compensation plan have the productivity-based incentive amount capped – which will affect the degree to which compensation will be impacted.5
Finally, in our experience, the market compensation per wRVU rate for APPs is often utilized in a different manner compared with physicians. Physician compensation plans typically directly utilize the market compensation per wRVU benchmark rate as a major incentive to drive compensation. For APPs, whose compensation plans are not as heavily incentivized as physician plans, organizations often just utilize market wRVUs and/or compensation per wRVU rates as a guide. Typically, APP plans allow for more significant guaranteed base salaries. Depending on the methodology used for each, this may limit the impact of any increases in APP compensation due to the changes.
Table 5 below highlights the estimated changes to survey benchmarks. See Column A to find the estimated change in compensation.
Table 5: Estimated Survey Benchmark Changes in Clinical Compensation and wRVUs
If an organization utilizes data on wRVU productivity targets to determine compensation using the pre-2021 survey data while calculating wRVUs using the 2021 wRVU schedule, this will result in higher payouts as APPs on incentive plans will meet or exceed the benchmarks at a much greater rate.
Similarly, if an organization uses the pre-2021 compensation per wRVU survey benchmarks while using the new 2021 values to calculate APP productivity, clinical compensation will increase as a result of the pre-adjusted compensation per wRVU rates.
These compensation change estimates are based only on the recalculations of the E&M wRVUs. This does not estimate other market factors that also drive compensation change. Additional factors include supply and demand, inflation, cost-of-living, changes in productivity and more. As with wRVUs, these factors can also vary significantly by specialty.
3. How will this impact APP compensation?
This depends on the structure of an organization’s existing APP compensation program and the degree of productivity incentive. It may have less of an impact than changes to physician compensation for a number of reasons:
- As noted previously, just over half (56%) of organizations use market wRVU data to adjust APP compensation.5
- Only 35% of organizations reported wRVUs for all APPs within the organization.5
- 42% are not tracking or reporting APP wRVUs at all.5
- 49% of organizations report having incentive plans for APPs with wRVUs being the most common component.5
Organizations incentivizing APPs based on wRVU productivity and utilizing national benchmarks to determine annual salaries and compensation per wRVU rates need to assess and understand how these changes to the benchmarks will impact APP compensation payout levels.
SullivanCotter reviewed several different compensation methodologies to estimate the impact on survey benchmarks. Considering the E&M code changes and assuming no modifications are made to compensation plan methodologies, we estimate the average clinical compensation for all APPs to increase by approximately 0.5%. This is compared to approximately 6% for physician compensation identified in Part I.
For organizations with APPs whose pay is structured more like physician compensation, it will be critical to understand the impact these changes will have on incentive plans – which is likely to be far greater than the average 0.5% suggested in this study.
4. If organizations utilize compensation per wRVU benchmarks for APPs, what should they expect with regard to the 2021 benchmarks?
For any group implementing the 2021 rate into their APP compensation plans, a fundamental understanding of how market benchmarks will change is important. This is especially true in some of the procedural specialties where APPs code a much higher number of E&M visits (compared to physicians who are more focused on the procedural codes). As a result, APPs will often see marked increases in wRVUs. It is important to monitor the unintentional impact on work effort for both APPs and physicians as clinicians adapt to the new weighting of professional encounters.
OTHER FACTORS TO CONSIDER WHEN ANALYZING COMPENSATION IMPACTS
As organizations continue to evaluate the impact of the 2021 Physician Fee Schedule, there are several additional factors to consider. These include:
- Are physician and APP compensation plans, incentive opportunities, and metrics aligned and will changes to one component impact the other?
- For specialties that include paid shift rates, are there additional incentives based on productivity?
- Does the organization pay physicians and APPs for virtual care visits that tie to E&M values? This could result in higher compensation for virtual care.
- Will the changes in CPT valuation for telemedicine be permanent or be adjusted after the end of the pandemic?
- CMS will also be adding G2212 as an add-on code for every 15 additional minutes of visit time. The assumptions and analysis above do not account for the changes in the distribution of E&M coding or increases in wRVUs due to these new codes.
- A wRVU increase does not automatically equate to an equal revenue reimbursement increase.
- CMS also applies an annual budget factor that caps the overall per wRVU reimbursement to avoid a significant increase in CMS payments. This can significantly increase the total percentage of revenue an organization receives that can be paid to physicians and APPs.
Sources:
1CMS Releases 2021 Physician Fee Schedule Rule. AAPA News Central. December 2, 2020. Accessed at: https://www.aapa.org/news-
central/2020/12/cms-releases-2021-physician-fee-schedule-rule/
2Proposed Policy, Payment and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2021. August 3, 2020. Centers for Medicare and Medicaid Services. Accessed at: https://www.cms.gov/newsroom/fact-sheets/proposed-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year-4
3Medicare Telemedicine Health Care Provider Fact Sheet. Centers for Medicare and Medicaid Services Fact Sheet. March 17, 2020. https://www. cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
4SullivanCotter Large Clinic® CPT Benchmark Study
5SullivanCotter 2020 Advanced Practice Provider Compensation and Productivity Survey
6SullivanCotter 2020 Physician Compensation and Productivity Survey
SullivanCotter offers advisory support and technology solutions to help your organization understand and respond to the potential impact of these changes.
To learn more, contact us at 888.739.7039 or info@sullivancotter.com
Q&A | Utilizing Technology to Engage the Clinical Workforce
Aligning clinical workforce compensation strategies with quality and efficiency goals
DOWNLOAD FULL ARTICLE
Healthcare continues to evolve at a rapid pace as the industry seeks to maintain financial sustainability and transform operations in the midst of post-COVID-19 recovery plans. This includes enhancing the quality of care, managing costs, improving patient access and satisfaction, and increasing physician and staff engagement to help achieve organizational goals. Market pressures are forcing organizations to develop new clinical capabilities as well as adapt their operations to perform more effectively under value-based reimbursement requirements. A key success factor in this evolution is the ability to align quality and efficiency goals with physician and advanced practice provider (APP) compensation strategies.
As pay practices continue to evolve, many organizations are looking to address the following questions:
- How can you ensure your compensation administration and performance management programs are engaging physicians and APPs in support of your cultural and organizational strategy?
- What tools and resources will help to enhance transparency in the reporting of performance to clinicians?
- What are the optimal communication, education and engagement processes to align performance around value-based metrics?
- How do these tools and resources help with recruitment and retention of the clinical workforce?
Compensation and performance management tools require transparency to build trust and reliability while also enhancing the clinical workforce’s ability to understand the process and the results.
Consistent measures, reporting, and expectations are foundational to building trust.
SullivanCotter consultants Kevin Wilson, Dan Iliff and Tom Trachtman recently answered questions on aligning physician and APP workforce performance — helping to uncover emerging trends, technologies and practices among high-performing hospitals, health systems and medical groups.
Why should healthcare organizations prioritize their compensation and performance programs during this transition?
DAN: Whether your organization is a single specialty independent medical group or one of the largest health systems in the country, success is reliant on the performance of your clinical workforce. As with any employee, in any industry, compensation and work expectations are two important variables. When appropriately designed and aligned, compensation plans play a vital role in helping to motivate this workforce and achieve organizational objectives. These variables are also important in clinical staff satisfaction and retention.
Physicians and APPs often express dissatisfaction when they do not fully understand their compensation plans, lack insight into how they are being measured, or do not have faith in the reporting system. This is becoming more common with the increasing prevalence of value-based pay components. This lack of transparency can leave them feeling disengaged and may contribute to turnover.
KEVIN: Agreed, Dan makes an important point. An effective compensation strategy is critical to engage and align the clinical workforce to achieve targeted performance. The importance of alignment is growing in the
transition to value-based care as organizations integrate more non-productivity metrics into compensation plans to help improve access, quality of care, service and affordability. Historically, physicians and APPs have lacked faith in the accuracy of reported non-productivity metrics. In order to reach desired outcomes and results, the administration, management and reporting process must be comprehensive and transparent enough to truly engage physicians and APPs. Regardless of the size or scope of your operations, a more transparent view into how physicians and APPs are performing and being paid is critical. This requires access to timely, accurate and actionable data in an understandable format. A comprehensive performance management program and process supported by innovative technology and reporting can help to achieve this.
What are some of the common administrative pain points hospitals, health systems and medical groups are experiencing as they try to support the engagement and alignment of a growing population of physicians and APPs within their organizations?
DAN: The way in which organizations measure and report physician and APP performance is often outdated and opaque. With a change in both the number and type of performance metrics being used, all of which help reflect a more balanced approach to performance, compensation programs are becoming increasingly complex and difficult to administer. Physicians and APPs often find the data difficult to understand, hard to verify and lacking in transparency. For these reasons, many organizations are struggling to effectively engage their clinicians in new pay-for-performance models that now include value-based metrics in addition to traditional productivity components.
According to SullivanCotter’s 2020 Physician Compensation and Productivity Survey, the prevalence of value/ quality incentives as a compensation plan component, which rewards performance on measures such as clinical quality, patient experience and access, hovers at or above 50% for all major specialty categories — primary care, medical, surgical and hospital-based. While reimbursement models continue to evolve and organizations are focused on incorporating more complex value-based components into their compensation programs, many organizations lack the internal processes and systems to efficiently track and manage multiple areas of performance. With multiple sources of information, this process can be both tedious and time-consuming, especially given the limited number of personnel assigned to the task.
Today, organizations often track performance relative to these new quality metrics in large and unwieldy offline spreadsheets. Not only do these spreadsheets create problems with version control, but error rates tend to increase as teams manually sift through endless rows of data. With nearly 90% of spreadsheets containing mistakes, this can prove costly as these errors can have a large impact on critical compensation and reporting functions.1 Additionally, there are the added complexities of data capture and validation across an increasing number of physicians, APPs and their associated sub-specialties. This complexity adds to the distrust that physicians and APPs often experience with these types of measures.
TOM: One of the most common issues I’ve seen related to this is delayed and incomplete production figures that lead to inaccurate performance results. Poor reporting makes it difficult for physicians and APPs to both track and trust what is being reported. Additionally, it makes it difficult for leadership to assess progress toward organizational goals. The lack of transparency doesn’t help to instill trust in the data. A large quantity of performance and productivity data must be properly merged, analyzed and validated from disparate systems before physicians, APPs, clinical leaders and managers can obtain and act upon the information they need. These limited reporting capabilities are a burden on the administrative staff responsible for delivering the information and helping to provide actionable insights.
Moreover, many organizations cite a lack of analytical talent available to properly evaluate the data they already have – and the COVID-19 pandemic may further this shortage. A recent report conducted by the Everest Group states that “75% of enterprises believe there will be a talent shortage for key roles in IT, analytics and special skills areas post-COVID-19…new skills gaps will emerge as a result of the structural changes in business occurring in response to the pandemic.”2 As health systems merge, consolidate and increase the number of physicians and APPs within the organization, the amount of data will only become more difficult to manage. Similarly, there must be control mechanisms in place to govern the data and ensure it maintains validity and relevance.
How can organizations develop a trusted performance management program that addresses and aligns a spectrum of needs for all key stakeholders — including leadership, physicians, APPs and administrative staff?
KEVIN: Clinical delivery structures are evolving and there should be a comprehensive process in place to administer, analyze and report on physician and APP performance and compensation across various levels of leadership. The first step is to consider the needs of each group of stakeholders:
Leadership
- Routine and consistent reporting with easy-to-consume information to assess progress towards organizational goals
- Actionable insights into drivers of performance at the organization, group and physician level
- Ability and capacity to focus on performance improvement efforts and coaching
Administration
- Accuracy, speed and reliability of performance and compensation analytics
- Alignment with internal partners
- Capacity and tools for deeper analysis
- Identification and reconciliation of issues
- Efficient utilization of technology to analyze real-time data to provide insight to leadership
Physicians and APPs
- A trusted and reliable source of truth for timely and efficient clinical compensation and performance management
- Easily accessible, current-state, performance results with clear action steps to help drive improvement
- Access to individual, peer and group performance in addition to patient-level detail
- Supporting resources (people, processes, technology) that enable physicians and APPs to make changes that can help improve results
How can technology be used to enable and provide greater value for your organization?
KEVIN: Alignment is important to building a trusted and reliable compensation and performance management program that engages clinicians. Along with the clinical workforce, leadership and administrators also require a clear understanding of expectations, progress and results. Without the ability to provide these insights in a timely fashion, these stakeholders are unable to effectively understand key drivers of performance and assess progress against goals. Building trust through transparency is key, and it leads to higher engagement, enhanced collaboration and clearer lines of communication. The expected outcomes should be clinically significant as well as easy to understand and measure.
With the addition of new quality incentives, a greater degree of “at-risk” compensation has become commonplace for physicians and APPs. Whether this “at-risk” compensation is based on panel size, access, clinical quality metrics or patient satisfaction, it is becoming common to have a component of compensation tied to performance. For primary care physicians, median quality incentive payments comprised 7.4% of total cash compensation in 2020.3 For medical and surgical specialists, this percentage is lower at 5.6% — although we expect to see growth as organizations work to further develop and refine these programs to ensure they have credible measurement and reporting systems in place before moving forward.3
DAN: I agree. High-performing organizations are constantly evolving and must be supported with tools and technology that can evolve with them. Technology is a platform for change at a time when change is inevitable. By providing access to clear and concise performance data all in one place, technology can serve as a single source of truth that combines administration, reporting and analytics capabilities into one system. The right technology can turn data into actionable insights, communicate goal definitions, benchmark performance, develop KPI reports and automate a number of data-related functions — all of which help to build trust and instill greater confidence in the data and reported results. Greater transparency can also play a critical role in improving engagement and aligning physicians and APPs with the mission and vision of the organization in which they work. Moreover, technology will enable physician leaders to better focus their efforts where it really counts — actively managing and coaching the clinical workforce.
What are the most important things to consider when assessing how technology can better support your performance management and compliance program?
DAN: New tools and technologies can allow your organization to streamline an increasingly complex communication, compensation and performance process by resolving inefficiencies in the way that data is collected, analyzed and reported. When assessing how technology can support these changes in relation to physician and APP compensation, performance and compliance, there are four key areas of functionality to consider:
- Performance management
- Productivity insights
- Compensation administration
- Contract lifecycle management
The first key area of functionality is performance management. Organizations must have a comprehensive system in place to communicate, measure, and drive performance while delivering actionable insights.
Once the key drivers of performance are identified, this understanding can then be translated into action and ultimately lead to improved results. Organizations must also provide the tools and support to help physicians and APPs improve performance while being mindful of not adding undue complexity or setting unrealistic expectations.
TOM: For example, imagine a scenario where physicians and APPs are compensated based on patient access. There has to be visibility into their schedules, time to next appointment, patient wait times and other components related to this metric. Without this visibility, there are limited fact-based insights to be gained.
The ability to properly assess performance and related compensation against defined targets and metrics is important to identifying best practices and improvement opportunities. Extensive built-in audit and reconciliation tools that help to ensure data integrity and improve the speed and accuracy of administration efforts exist in the marketplace today and can provide customized access and views tailored to the unique needs of leadership, physicians and administrators.
DAN: Another key piece of functionality relates to productivity insights. As a result of constantly changing wRVU schedules, evolving compensation models, billing reconciliation and other changes, physician and APP compensation and performance administration is multifaceted. Technology that automates the revenue and productivity data collection and analysis component of this process will yield immediate time savings for physicians, APPs and administrators. Additionally, it will allow physicians and APPs to be able to understand the reported data and have faith in the process. A system that allows you to review billing information in a central repository and assists with complex RVU functions such as sharing arrangements, scale conversion, modifier adjustments and non-billable credit information will greatly increase the speed and accuracy of a multitude of productivity assessments. The consistency and transparency of the process will also build trust with the physicians and APPs and ultimately creates time and credibility for your team to dedicate to more strategic initiatives.
The third area of focus is on compensation administration — or the communication of results. This is where a compensation program comes full circle through customized dashboards and reports that are tailored to
individual providers and administrators. By integrating data on compensation earned from all sources for all physicians and APPs in a central repository, technology will help streamline the reporting process and get the right data into the right hands at the right time. The timely delivery of accurate compensation results to the clinician strengthens trust and improves engagement. Whether you are an administrator facilitating monthly settlements or a physician or APP monitoring performance on specific metrics, these dashboards are the key to success and will help to track progress against organization-wide goals.
Lastly, ensuring that physician employment agreements align with system-wide compensation terms and payments remains a challenge for health care organizations nationwide. Integrating an automated contract
lifecycle management solution that will provide your organization with an accurate and comprehensive view of clinical employment contracts and obligations across the organization in real-time helps to support compliance and ease of administration while also providing transparency and greater access to the clinicians.
The ideal technology solution brings all four of these components together to equip your organization with a more transparent, accurate and timely view of individual, group and system performance. physicians and leadership with the information they need to reliably inform performance and drive desired outcomes. A strong technology platform can act as the cornerstone to help facilitate change. Similar to how EHRs revolutionized care delivery, a mature compensation and performance infrastructure can help to revolutionize how performance is measured and communicated.
What are the next steps for organizations considering the implementation of a new compensation and performance management system?
TOM: Compensation and performance programs are constantly evolving in today’s dynamic health care marketplace and organizations will continue to adapt as operations grow more complex. They require scalable solutions to help streamline the compensation administration process while also providing physicians and leadership with the information they need to reliably inform performance and drive desired outcomes. A strong technology platform can act as the cornerstone to help facilitate change. Similar to how EHRs revolutionized care delivery, a mature compensation and performance infrastructure can help to revolutionize how performance is measured and communicated.
DAN: The specific actions your team should consider include:
- Identify key stakeholders through a holistic analysis of your compensation and performance program
- Aggregate and organize pain points across stakeholders to identify their root cause
- Acknowledge gaps in technology in order to meet the needs of all stakeholders
- Determine the functionality required to assess, analyze and report on physician and APP performance
- Evaluate the technology options available and how respective platforms can help advance your organization’s performance management programs
SullivanCotter’s Provider Performance Management Technology™
Provider Performance Management Technology™ (PPMT™) is an industry-first, cloud-based solution that enables clinician engagement through transparent performance-based compensation administration, contract management, and reporting and analytical capabilities.
Utilizing best-in-class technology and decades of physician compensation and health care expertise, PPMT™ is designed to support organizations in the transition from volume to value. PPMT™ is offered as part of a comprehensive portfolio of advisory, information and technology services to address client needs.
As a trusted partner in compensation and performance management, reach out to SullivanCotter to learn more about our comprehensive Provider Performance Management Technology™ and our suite of clinical workforce advisory services.
Sources:
- 1Olshan, Jeremy. (2013). 88% of Spreadsheets Have Errors. MarketWatch. Retrieved from https://www.marketwatch.com/story/88-of-spreadsheets-have-errors-2013-04-17
- 2The Everest Group. (2020). 75% of Enterprises Bracing for Widening IT & Analytics Talent Shortage Despite Recession. Retrieved from https://www.everestgrp.
com/2020-08-75-of-enterprises-bracing-for-widening-it-analytics-talent-shortage-despite-recession-press-release-.htmlhttps://hitconsultant.net/2019/10/16/health-it-staffing-shortage-crisis/#.YGtEaehKiUk - 3SullivanCotter 2020 Physician Compensation and Productivity Survey Report
Modern Healthcare | Physician Compensation Plateaus During Pandemic
Protecting physician compensation during the COVID-19 pandemic
While many healthcare organizations continue to undergo post-pandemic financial and operational recovery planning, maintaining the broader workforce remains a top priority. Although physician compensation may have been expected to drop over the course of the last year due to a major decline in patient volumes and the cancellation of elective procedures during the shutdown, the majority of hospitals and health systems implemented to protect physician compensation to some degree.
Featured in a July 2021 edition of Modern Healthcare, SullivanCotter helps to evaluate how compensation evolved during the COVID-19 pandemic, which pay actions organizations implemented in response, and how to move forward with evaluating pay programs for 2021 and beyond. Organizations will now need reassess physician pay models in light of recent events to help maintain operations and support future sustainability while paying close attention to newly-released 2021 benchmarks and effectively adjusting for months most affected by the pandemic.
READ FULL ARTICLE
Clinical Workforce Technology Solutions | Webinar Series
To help healthcare organizations address increasingly dynamic clinical workforce requirements, SullivanCotter continues to strengthen our innovative suite of technology, survey and data products.
Join us as we feature some of our newest product enhancements and demonstrate how you can leverage data-driven insights to identify physician market demand, interactively analyze workforce benchmarks, administer compensation and performance management programs, and automate the physician contract lifecycle to better support your care team and population health initiatives.
As we continue to refine our product roadmap, we’d love the opportunity to hear your feedback on various features and functionality, proposed enhancements, and key clinical workforce challenges that your organization is facing.
Session 1: Benchmarks360™
Tuesday, July 27 | 12:00pm-12:45pm CT
Powered by SullivanCotter’s proprietary survey data and research, Benchmarks360™ is a suite of intelligent, web-based products that enables healthcare organizations to analyze and visualize compensation, clinical productivity, and workforce perceptions.
What's New?
-
- Complimentary access to survey participants
- APP Utilization and Perceptions Manager module
- Pay Practices Manager module
- Standard, Plus and Pro versions now available for the Workforce Compensation and Clinical Productivity Manager module
REGISTER TO ATTEND >
SESSION 2: Physician Needs Assessment
Tuesday, August 3 | 12:00pm-12:45pm CT
SullivanCotter’s Physician Needs Assessment is an interactive cloud-based application that delivers accurate and actionable data-driven insights to help organizations identify, monitor and respond to changing service needs and physician and advanced practice provider staffing requirements in the communities they serve.
What's New?
- Market-specific assessment to provide accurate and detailed reporting of physician supply and demand
- Interactive mapping tool with the ability to select specific zip codes for strategic consideration
- Comprehensive customizable reports with 5-year rolling projections
REGISTER TO ATTEND >
SESSION 3: Provider Performance Management Technology™
Tuesday, August 10 | 12:00pm-12:45pm CT
With Provider Performance Management Technology™, organizations can build trust and engagement with the clinical workforce through actionable and transparent performance-based compensation administration, contract management, reporting and analytical capabilities.
What's New?
- Panel attribution and compensation management capabilities
- Automated clinical draw calculations and payments
- Automated split-role compensation calculations
- Full-scale physician contract lifecycle management
REGISTER TO ATTEND >
PRESS RELEASE | SullivanCotter’s Not-for-Profit Practice Welcomes Amanda Wethington
Supporting not-for-profit organizations in the attraction, retention and motivation of high-caliber talent
June 29, 2021 – Chicago – SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the health care industry and not-for-profit sector, welcomes new Principal Amanda Wethington to the firm’s Not-for-Profit Practice. Joining practice leader Nanci Hibschman, Amanda will help to support SullivanCotter as it continues to expand its advisory services, proprietary survey data and insights to better serve the not-for-profit sector nationwide – including private and community foundations, higher education, policy and research institutes, trade and professional associations, and other service and charitable organizations.
With nearly 20 years of experience delivering comprehensive workforce compensation and performance solutions across a number of industries, Amanda leverages data-driven insights to help organizations align total rewards, recognition, and talent management programs. She works to solve the unique challenges that not-for-profit organizations face in the attraction, retention, and motivation of high-caliber talent.
She serves as a close advisor to boards and leadership on executive and employee total rewards programs with a focus on improving the design, development and implementation of compensation and performance management programs to enhance alignment with an organization’s mission, vision and values.
“In today’s complex operating environment, high-performing not-for-profit organizations require increasingly competitive compensation, benefits and talent strategies in order to stay ahead of the curve. Amanda’s in-depth experience in delivering effective total rewards strategies, including diversity, equity and inclusion initiatives, will serve our clients well as they continue to look for guidance on developing innovative programs that support key organizational objectives,” said Nanci Hibschman, Managing Principal and Not-for-Profit Practice Leader, SullivanCotter.
Prior to joining SullivanCotter, Amanda led the Workforce Rewards Team as a Senior Principal at a global management consulting firm. She also spent 10 years working in human resources and compensation at Hyatt Hotels Corporation.
About SullivanCotter
SullivanCotter partners with health care and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON NEWSDIRECT
Advanced Practice Provider Leadership Structures
The Evolution of a Well-Defined Advanced Practice Provider Leadership Structure
READ FULL ARTICLE
Featured in AAPL's Physician Leadership Journal
Advanced practice provider leadership is critical to the optimization of the growing APP workforce.
COVID-19 has accelerated the financial and operational challenges facing the health care industry and organizations are reevaluating current processes and structures. As a result of this pandemic, some health systems and medical groups are planning for an increasingly uncertain future. These changes have also presented the opportunity to design more effective care delivery models, right-size cost structures, and streamline organizational processes to enhance financial sustainability going forward.
Prior to the pandemic, many hospitals and health systems had begun to prioritize the integration, optimization and engagement of their advanced practice provider (APP) workforce as a strategy to enhance organizational performance and support the transition to value-based care. In response to COVID-19, many organizations are utilizing their APPs to support operations. This has, in many cases, helped to accelerate the optimization of these clinicians.
As one of the fastest-growing workforces in health care, APPs constitute, on average, more than one-third of an organization’s clinical workforce. APP leaders are critical to the organization and optimization of this workforce. The presence of a well-defined advanced practice provider leadership structure can drive organizational performance and support a comprehensive APP workforce strategy – which can help to improve access, increase revenue and reduce costs. Understanding the evolution of APP leadership positions at the top, clinical, managerial and functional levels, along with their different roles and responsibilities, can serve as a roadmap for organizations as they continue to build out and develop their own APP structures and programs.
PRESS RELEASE | Sophisticated Compensation Enhancements Added to PPMT™
SullivanCotter's comprehensive physician compensation software now includes innovative automation enhancements for its new Clinician Pay feature
June 15, 2021 – Chicago – SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, announces the addition of highly-anticipated new compensation automation enhancements to its growing physician compensation software solution – Provider Performance Management TechnologyTM (PPMT).
With the new Clinician Pay feature, PPMT™ now enables users to streamline the compensation management process by automating clinical draw calculations and payments based on current performance and organization-defined criteria. It offers flexible and sophisticated rules for the draw calculations that are easily maintained by key administrative stakeholders and can be managed throughout the year.
“Determining clinician draw for the upcoming year is a significant and burdensome time investment for compensation program administrators. Most often, these calculations are done manually via spreadsheets – which can greatly increase the risk of error. Using PPMT™, organizations can now automate the production of accurate and reliable draw and other pay calculations within one system”, said Shelly Slowiak, Director, Product Support, PPMT™, SullivanCotter.
New split role compensation automation eliminates the need to manually determine clinical and non-clinical pay components by providing visibility into performance and compensation for different roles while also allowing administrators to view aggregate compensation for each individual clinician.
“In order to provide the best care for patients, a growing number of physicians are specializing in multiple service areas with varying compensation arrangements. This often requires greater attention and additional analysis from an already overextended compensation team. PPMT™ can ease the administrative burden by effectively automating and providing consistent compensation calculations for each service area”, said David Schwietz, Chief Information Officer, SullivanCotter.
Designed to address a spectrum of physician, leadership and other key stakeholder needs, PPMT™ combines years of health care compensation insight and expertise with an intuitive and automated technology platform to help drive provider performance and support the transition from volume- to value-based care.
For more information on these enhancements or our entire suite of Provider Performance Management Technology™, visit www.sullivancotter.com/PPMT or contact us at 888.739.7039.
About SullivanCotter
SullivanCotter partners with healthcare and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON NEWSDIRECT
Advanced Practice Provider Utilization and Compensation | Case Study
Optimizing advanced practice provider utilization to increase retention and engagement
Featuring a case study from a large academic medical center
DOWNLOAD FULL ARTICLE
At a time when healthcare organizations remain focused on pandemic-related financial and care delivery challenges, there is an acute need to engage and retain the clinical workforce by reducing burnout and unexpected turnover – and how advanced practice provider utilization within the care team can have a significant impact on both.
As organizations look for better ways to support their growing APP workforce, they require an intentional approach that aligns compensation design more closely with the goals of care team optimization in order to reduce costs and improve team performance.
In an article written by SullivanCotter and published by the American Association of Provider Compensation Professionals, learn more about how one organization set the stage for optimal APP utilization and care team delivery by also addressing important compensation issues at the same time.
PRESS RELEASE | SullivanCotter Names New Independent Members to its Board of Directors
New Independent Directors will play a pivotal role in providing the additional insight, experience and external perspective needed to support business strategy, ensure organizational growth and maintain independence
May 18, 2021 – Chicago –SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the health care industry and not-for-profit sector, is pleased to announce the addition of five independent advisors to the firm’s Board of Directors.
“While our firm continues to expand and evolve amidst a number of unprecedented industry changes, advancing our strategic plan to help better serve the dynamic and unique needs of our clients remains a top priority. By inviting an accomplished group of Independent Directors to join our Board, we hope to leverage their strategic thinking, market knowledge and many years of combined experience as we move forward into 2021 and beyond,” said Ted Chien, President and CEO, SullivanCotter.
In an effort to prioritize best practices in governance, information technology, financial and human capital development, and diversity, equity and inclusion, SullivanCotter welcomes the following Independent Directors to the Board:
- Gina Alexander – Current Chief Financial Officer for AlixaRx, a privately-held, technology-enabled pharmacy services company serving the long-term care and corrections market.
- Brian Dunn – An experienced consultant who retired as the Chairman of McLagan and the CEO of Performance, Reward and Talent at Aon Consulting.
- Frances Ferguson – An accomplished C-Suite executive with more than 25 years of experience who most recently served as Group Executive, Managing Director and the Chief Administrative Officer of the Financial Markets and Treasury Services Sector operations at BNY Mellon Bank.
- Paul Keckley – Managing Editor of The Keckley Report, a health care policy analyst and widely known industry expert who advises health care organizations on long-term growth, sustainability, and advocacy strategies.
- Robert Oberrender – A decorated financial executive who recently retired as the Chief Investment Officer and Treasurer of UnitedHealth Group in October 2018.
As SullivanCotter continues to innovate through its performance-focused advisory services and growing suite of technology, survey and data products, these new members will play a pivotal role in providing the additional insight, experience and external perspective needed to support business strategy, ensure organizational growth and maintain independence.
To learn more about SullivanCotter’s Board of Directors, visit us at SullivanCotter.com or call 888.739.7039.
About SullivanCotter
SullivanCotter partners with health care and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.