SullivanCotter’s Provider Affiliation and Optimization focuses on identifying, quantifying, and optimizing physician and advanced practice provider (APP) performance to improve provider productivity, engagement, financial results, staffing ratios, and overall efficiencies.
Our goal is to assess and optimize physician enterprise performance within health systems to improve patient outcomes, boost physician and APP care team collaboration, and support collective value-based initiatives and reimbursement opportunities
Provider Affiliation and Optimization services encompass two types of work: Affiliation Services and Performance Optimization.
Affiliation Services and Performance Optimization work in concert as organizations seek to determine whether their investments in provider affiliations are meeting a market need, yielding optimal performance, and maximizing return on investment.
Affiliation Services are critical to a health system’s partnerships with providers. There is a continuum of affiliation models ranging from low levels of affiliation to full practice integration and employment, as illustrated in the same range of models set forth below.
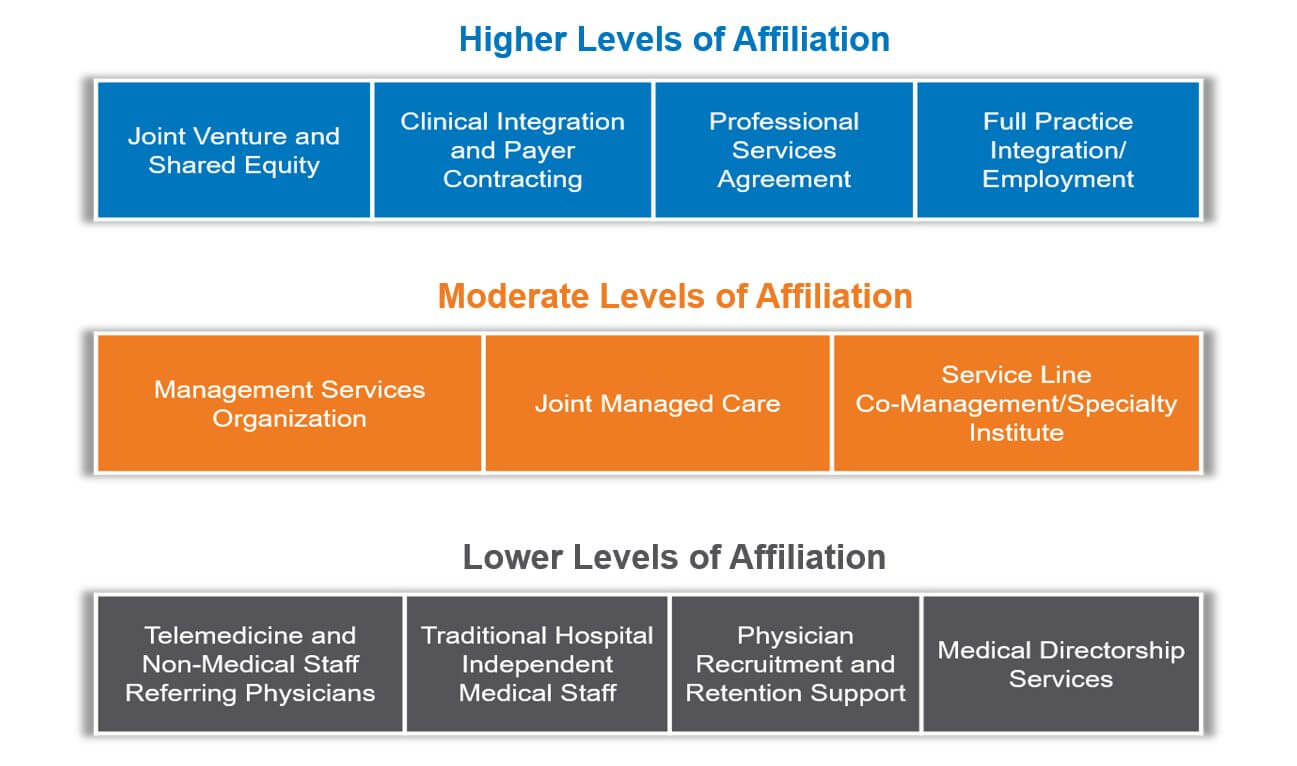
SullivanCotter has extensive experience in the assessment, development, and implementation of these and other affiliation relationships between physicians, medical groups, and hospitals.
We enhance affiliation relationships by providing:
- Assessments on a wide range of physician affiliation models, including professional services agreements, co-management arrangements, joint ventures, clinical integration, and more
- Pre-affiliation due diligence (including potential review or update to provider needs assessments and workforce plans)
- Model selection (including an assessment to find the proper affiliation framework and recommended leading practice affiliation model characteristics, with tailored compensation and core performance expectations for your organization’s strategic alignment and accountability needs)
- Deal structuring (including aligning new or revised aligned compensation and benefits arrangements)
- Negotiation (including third-party facilitation or independent advising to one or more of the parties assessing new or revised affiliation relationships)
- Management and governance review assistance (including presentation of proposed terms, pro forma development, and other proposed performance requirements)
- Post-affiliation implementation (including implementation assistance, performance improvement assistance, performance management oversight and other facilitated communication and provider management assistance)
- Insight into high-demand specialties such as anesthesiology, radiology, and more
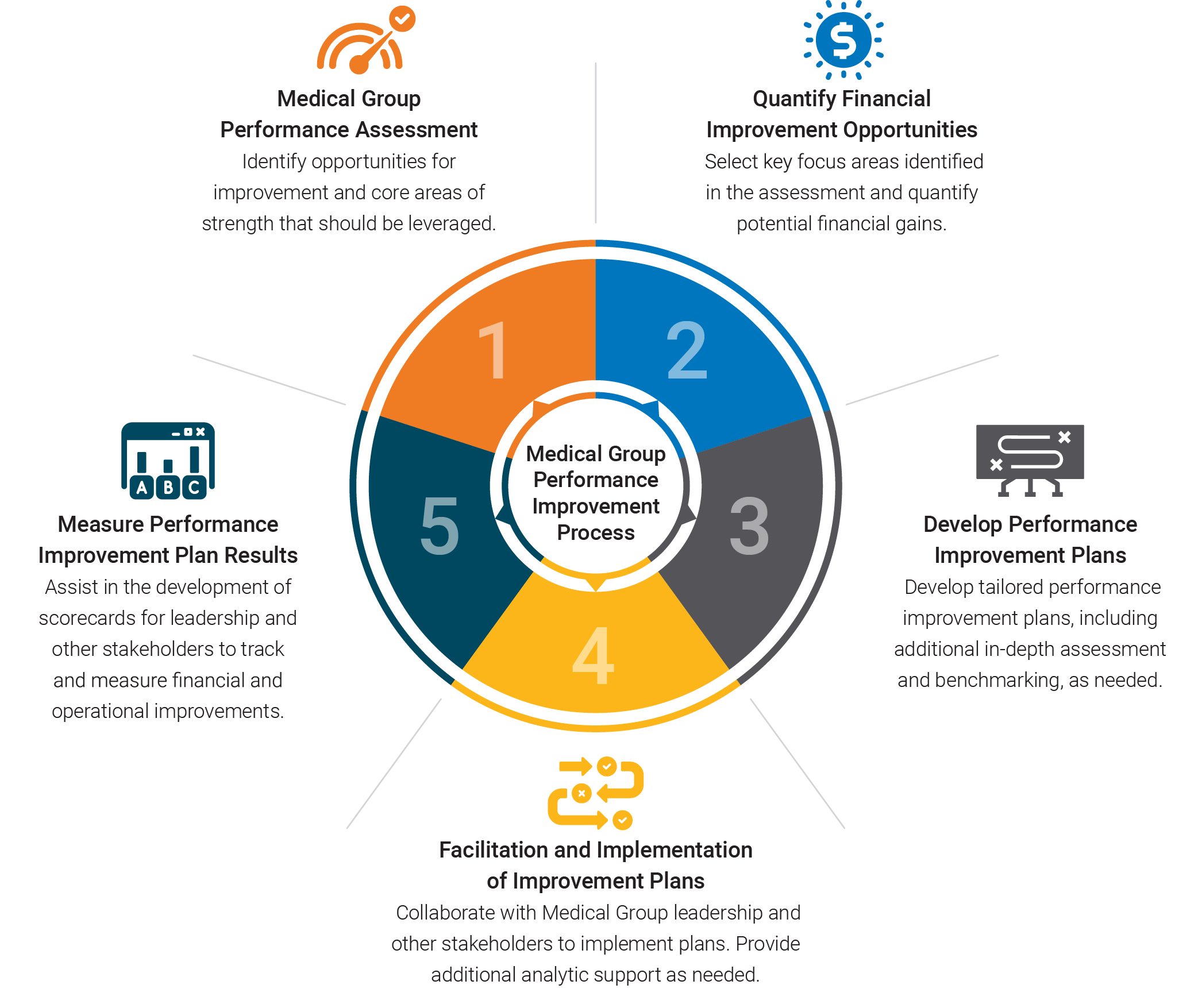
Performance Optimization is critical to the success of a health system’s business model and is based on a 5-step Performance Improvement Process. The comprehensive steps in the Performance Improvement Process include:
The Client Problems We Solve:
- Growth: Many health systems are currently experiencing stagnant market share growth. We provide clear strategies related to acquisitions, joint ventures, and other affiliation approaches to drive growth and increase provider engagement.
- Physician/Health System Alignment: Successful physician alignment with health systems and hospitals is necessary to improve patient outcomes, enhance patient access, and support value-based initiatives. We help clients select, develop and implement the affiliation model(s) that best meet their objectives.
- Financial Performance: With declining reimbursement and increasing costs per provider, health systems are under substantial pressure to find new ways to remain financially sustainable. Our performance optimization services help health systems assess, develop and implement targeted improvement solutions to improve financial performance.
- Operational Performance: Inadequate operational designs negatively affect medical group and/or service line performance. We support health systems with operational improvement solutions that promote provider productivity and engagement, improved patient access, revenue cycle improvements, staffing and cost efficiencies and overall medical group performance.
- Care Delivery Optimization: Sustainable models of care increase care delivery teams’ ability to enhance alignment, improve productivity, expand market share, control service line costs, drive financial margins and improve quality outcomes within a collaborative framework.
- Recruitment: Existing workforce plans evaluate current and future capacity needs to ensure the right long-term clinical staffing. We work with clients to develop and execute these workforce plans for actionable results.
RELATED CONTENT
Trends in Physician-Hospital Affiliation Strategies
ARTICLE | Practice Acquisition Strategy and COVID-19: Adjusting for the New Normal
ARTICLE | Optimizing Care Delivery in Response to COVID-19
CASE STUDY | The Key Role of APPs in Today’s New Normal – The Stanford Story
Provider Needs Assessment
Introducing SullivanCotter’s interactive
cloud-based application
As hospitals and health systems look to support growth and reassess cost and efficiency concerns in a rapidly evolving marketplace, access to current and projected market-specific physician supply and demand data is critical.
SullivanCotter helps organizations assess and develop a wide range of physician affiliation models - including those along the sample continuum below - from highly integrated to more modestly affiliated:
- Telemedicine and Area Referring Physicians
- Traditional Hospital Independent Medical Staff
- On-Call Coverage Relationships
- Physician Recruitment and Retention Support
- Medical Directorship and Other Professional Services Agreements
- Management Services Organization (MSO)/Practice Management
- Joint Managed Care (with lower levels of risk)
- Specialty Institute /Service Line and Program Co-Management
- Joint Venture and Shared Equity Relationships
- Clinical Integration and Payer Contracting (with higher levels of risk)
- Exclusive Foundation/Professional Services Agreement
- Full Practice Integration/Employment
Learn more about enhancing physician-hospital affiliation relationships within your organization
Related Resources
Press Release | SullivanCotter Releases Results for 2025 Health Care Compensation Surveys
With participation from more than 90% of the nation’s largest 200 health care organizations, these surveys represent one of the most comprehensive sources of health care compensation and workforce benchmarks available.
FORBES | Aligning Clinical Contracts with Value-Based Care
Your clinical workforce is critical to achieving the goals of value-based care. For many health systems, however, this strategy falls apart at the contract, compensation, and incentive level. Learn more from SullivanCotter's Ted Chien on how to adapt!
On-Demand Webinar | Beyond the Org Chart
Get the latest insights from our experts on transforming your health system design through data-driven organization design!