The modifications to the 2021 Physician Fee Schedule will impact Work RVU values and reduce Medicare reimbursement rates.
Is your organization prepared?
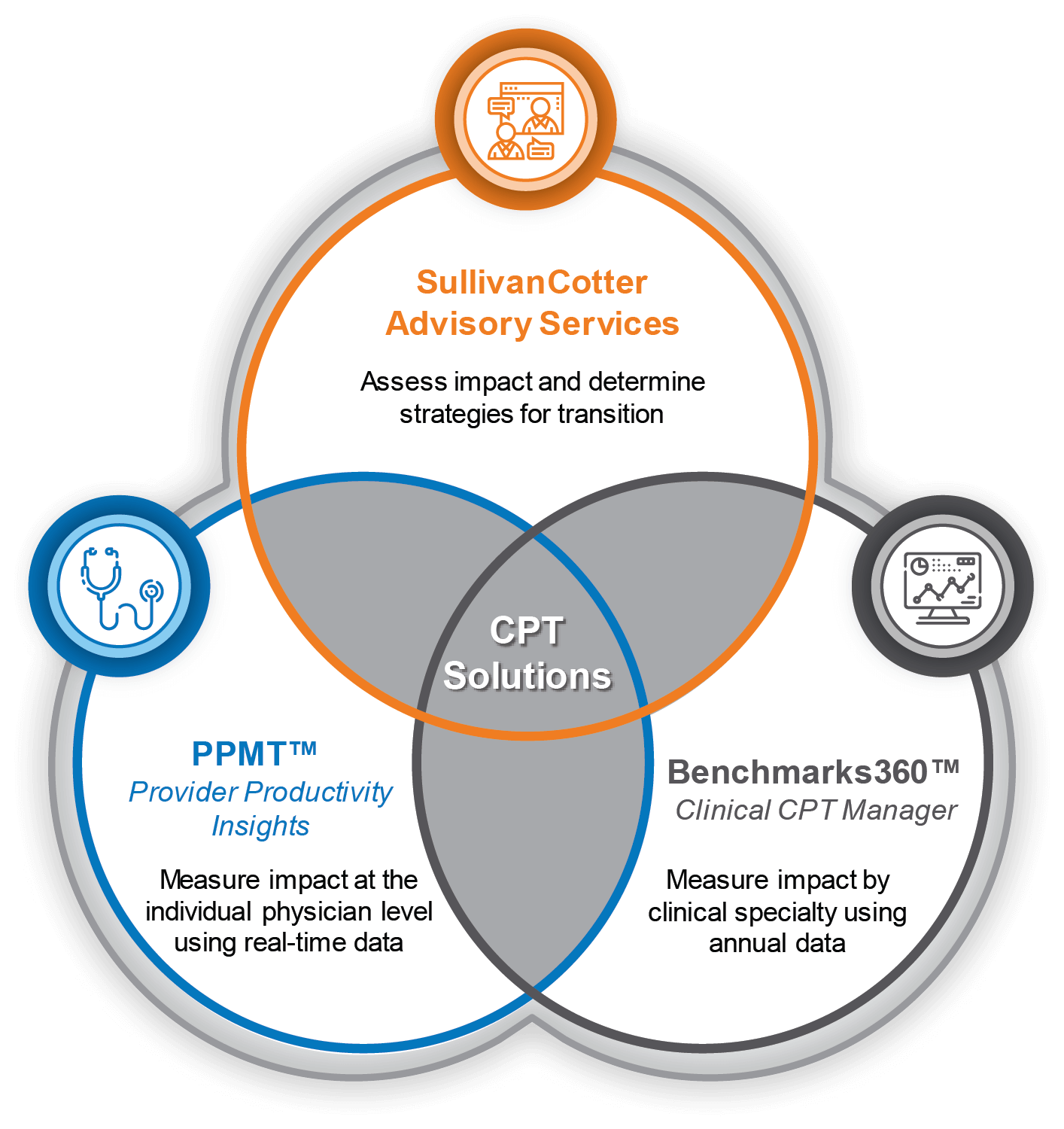
SullivanCotter CPT Solutions
On December 1, 2020, the Centers for Medicare & Medicaid Services (CMS) finalized its 2021 Physician Fee Schedule changes to the Evaluation & Management (E&M) codes, as well as other outpatient equivalent visit codes for OB and ESRD, and corresponding work RVU values to recognize increased work effort for office visits. These changes will have material implications on professional services reimbursement and physician and advanced practice provider (APP) compensation going forward.
The health care industry has not seen broad work RVU changes of this magnitude in well over a decade, so it will be critical for organizations using productivity-based plans to understand the impact of these changes on payor reimbursement, reported physician and APP productivity levels, employed and independent physician compensation arrangements and budgets, and to identify potential fair market value and commercial reasonableness implications.
Learn more about the changes to the 2021 Physician Fee Schedule >
Provider Performance Management Technology™
Provider Productivity Insights
- Analyze impact of changes to CPT codes and work RVUs against annual CMS scale conversion
- Load real-time data for ongoing review and analysis of work RVU productivity
- Work RVU and CPT code level productivity reporting capabilities at the organizational and individual physician or APP level
- Compare individual physician or APP work RVU productivity against any market-leading benchmarks survey
Benchmarks360™
Clinical CPT Manager
- Analyze and compare your organization’s CPT coding distribution at the specialty level against national physician and APP benchmarks including work RVU and CPT level volumes
- Visualize trends in annual coding profiles and benchmarking data
- Model impact of volume and full-time equivalent changes
- Leverage automation to remove data and reporting errors
- Customize views of coding details for clearer insights and custom analyses
SullivanCotter’s CPT Advisory Services
- Guidance on the changes and important considerations relative to 2021 planning and beyond
- Market insight and perspective on how other organizations are addressing the changes
- Assistance in assessing the anticipated impacts, including technology solutions available to help in that analysis
- Help understanding and identifying the potential implications of fee schedule changes on current fair market value standards and processes
RELATED CONTENT
ARTICLE | 2022 Physician Fee Schedule: Understanding Changes to Split/Shared Visits
ARTICLE | 2021 E&M CPT Codes: Understanding the Impact on Physician Compensation
INFOGRAPHIC | Considerations for Addressing the 2021 E&M wRVU Changes
ARTICLE | Navigating Change: Implications of the 2021 Physician Fee Schedule Changes
Benchmarks360™
Powered by SullivanCotter’s proprietary benchmarking information, Benchmarks360™ is a suite of intelligent, web-based products that enables health care organizations to analyze and visualize workforce compensation and clinical productivity.
Provider Performance Management Technology™
An industry-first, cloud-based solution that enables provider engagement through transparent performance-based compensation administration, reporting and analytical capabilities.
Address the impact of CPT code changes on compensation and productivity
Related Resources
INFOGRAPHIC | Value-Based Performance Measures
Optimize reimbursement by aligning physician compensation more closely with value-based payer incentives. Learn more from our latest infographic!
Forbes | Fixing Health Equity and Access: Is Collaboration the Answer?
The industry is experiencing large gaps in care and patient access amidst ongoing labor shortages – all of which are hindering health equity programs. Learn more about how not-for-profit health systems can band together to enact real change from SullivanCotter's President and CEO, Ted Chien.
INFOGRAPHIC | APP Unrestricted On-Call Pay
As organizations strive to meet patient demand, one premium pay practice that continues to receive attention is on-call pay. Establishing an effective call pay approach for advanced practice providers can help to support care coverage needs, improve patient access, and maintain effective throughput.