APPs: 2021 Evaluation and Management CPT Codes
Part II: Understanding the Impact on Advanced Practice Providers
DOWNLOAD FULL ARTICLE
RELATED CONTENT:
PART I | 2021 E&M CPT Code Changes: Understanding the Impact on Physician Compensation
INFOGRAPHIC | Considerations for Addressing the 2021 E&M Work RVU Changes
ARTICLE | Navigating Change: Implications of the 2021 Physician Fee Schedule
SullivanCotter’s CPT Advisory Services and Technology Solutions
BACKGROUND
Every year, the Centers for Medicare and Medicaid Services (CMS) evaluates the recommendations of the American Medical Association’s Relative Value System Update Committee and conducts its own review of the Work Relative Value Unit (wRVU) values associated with each Current Procedural Terminology (CPT) code to determine if revisions are needed based on the time, skill, training and intensity necessary to perform each service. The degree of change varies from year to year, and the impact on individual specialties depends on which codes are modified and the extent to which the codes are adjusted.
CURRENT SITUATION
At the end of 2019, CMS proposed widespread modifications to a subset of the Evaluation and Management (E&M) CPT codes (99201-99215) that include face-to-face office visits and other outpatient services for new or established patients. The goal of the adjustments is to provide an increase in certain wRVU values to address added responsibilities clinicians have absorbed over the last five years, reduce documentation requirements, recognize extended patient visits, and account for qualified, severe or complex chronic conditions. On December 1, 2020, CMS finalized the 2021 Physician Fee Schedule – which went into effect on January 1, 2021.
Additionally, in response to COVID-19, CMS has implemented new guidance as it relates to telehealth services. Although it is unknown whether these CPT code changes will be maintained or altered as the pandemic subsides, the agency has indicated a desire to make longstanding revisions to telehealth visit valuations. While the 2021 Physician Fee Schedule final rule permanently expanded some of the telehealth changes for rural communities, the adoption of the telehealth changes has not been identified as permanent.
In Part I of this series, SullivanCotter explored the impact of the E&M code changes on physician compensation and productivity levels as well as other implications health care organizations must be mindful of as they plan physician compensation for 2021 and beyond. For additional background, Part I also included a detailed summary of the final changes – including greater insight into the “Patients Over Paperwork” goal, the results of a work-effort/time-study commissioned by CMS, and two related add-on codes.
As we continue to assess how these changes affect the clinical workforce, Part II in this series reviews the impact on advanced practice providers (APPs).
ADDRESSING THE IMPACT ON ADVANCED PRACTICE PROVIDERS
Based on the overlapping scope of services performed by APPs and physicians, CMS modifications to CPT code valuations will impact both APPs and physicians. At a broad level, these changes include:
- An increase in wRVUs for most office-visit E&M CPT codes due to added responsibilities clinicians have absorbed over the last five years.
- A 3.3% reduction in the Medicare conversion factor (now $34.89) for physician fee schedule payments to maintain budget neutrality that impacts all E&M services no matter who provided the service.
- An add-on code to recognize extended office-visit time.
Due to the differences in practice patterns between APPs and physicians, there will be some variation in how the changes will impact APPs as compared to physicians. The differences may include the following factors:
- APPs often perform a greater amount of non-billable work and provide services covered under a global visit.
- APPs may see lower acuity patients in some specialties or settings.
- In our analysis of reported CPT data, APPs in surgical specialties report E&M services (e.g. office visits) as a greater proportion of their overall work compared with physicians who report a relatively greater proportion of procedures and surgeries.
Additionally, there are some APP-specific provisions that may affect scope of practice:
- Effective as of January 1, 2021, Medicare now permits physician assistants (PAs) to perform diagnostic tests in accordance with supervisory requirements outlined in state law rather than in Medicare’s general supervision requirements. This change means that PAs are no longer subject to two sets of requirements as Medicare now defers to state policy instead. This helps to reduce administrative burden and potential confusion within organizations about which regulations to follow.1
- The rule for 2021 allows all APPs (APRNs and PAs) to supervise the performance of diagnostic tests in accordance with their state’s scope of practice. Previously, only physicians were authorized to do so. The ability of APPs to be able to perform diagnostic tests will likely have an impact on APP procedural specialties like interventional radiology and some medical specialties such as cardiology and gastroenterology.2
As healthcare organizations absorb these changes and plan for what lies ahead, there are a number of practical implications for APP productivity and compensation to keep in mind. This article helps organizations to understand and address the impact on APP productivity levels in various specialties, temporary changes to telehealth codes, and unintended consequences for APP productivity-based incentive plans. It also highlights other variables that could influence the assessment of APP productivity – such as survey benchmarks and how to utilize these going forward.
WORK RVU ADJUSTMENTS
The impact of the wRVU changes may result in material shifts in wRVU productivity for APPs. According to SullivanCotter’s 2020 Advanced Practice Provider Compensation and Pay Practices Survey, over 40% of APPs work in office-based specialties and ambulatory clinics.
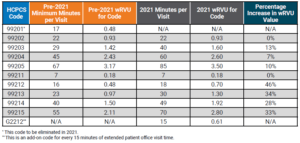
Table 1 below compares the pre-2021 E&M code time allocation and wRVUs to the January 2021 changes.
Note that the established office-visit codes 99212-99215, which are the most frequently used office-visit codes, show the most significant increases between 28%-46%. To balance CMS’ expenditures, the 2021 conversion factor, which is multiplied by total RVUs to determine Medicare payments to physicians and APPs, has dropped by 3.3% from $36.09 to $34.89. SullivanCotter notes that approximately half of the rate reduction mitigation is designated only for the 2021 calendar year as a result of the Consolidated Appropriations Act of 2021 – meaning an additional conversion factor reduction looms for 2022.
This change impacts all clinicians regardless of specialty and, combined with the E&M wRVU increases, creates a redistribution of federal payer reimbursement from proceduralists and hospital-based specialties to cognitive specialties.
Table 1: Time Allocations and wRVUs Adjustments: Current Versus 2021
Additionally, there are CPT code changes related to COVID-19 that will impact both physician and APP compensation and productivity. In March 2020, CMS expanded the Medicare telehealth coverage waiver to enable beneficiaries to receive a wider range of health care services from clinicians without having to travel to a health care facility. The announcement expanded previous telehealth coverage for beneficiaries living in rural areas who were able to receive care at a local facility with a clinician from a remote area.3
Under the new provisions, all beneficiaries are able to receive telehealth coverage. Effective March 2020, telehealth services were paid under the Medicare Physician Fee Schedule at the same rate as in-person services.
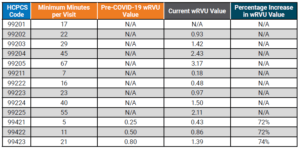
Table 2 below compares the pre-COVID-19 E&M code time allocation and wRVUs to the changes made in March 2020. It is unclear how long CMS plans to keep the expanded rates in place.
Table 2: Telehealth wRVU Adjustments: Results of 2020 Waivers
THREE IMPORTANT POTENTIAL IMPACTS TO APP PRODUCTIVITY LEVELS AND RESULTING COMPENSATION AND BENCHMARK MEASUREMENTS
1. How will the 2021 wRVU changes impact the measurement of APP productivity?
This common question is complex for APPs given that productivity benchmarks have generally been difficult to collect and interpret due to the wide variation in how APPs are utilized – even within the same specialty. Historically, productivity data has been absent, inconsistent or inaccessible due to the variety of billing practices used to capture APP work effort including shared visits and incident-to billing. Additionally, APPs often perform more non-revenue generating work compared to physicians in the same specialty (e.g., global visits) – contributing to inconsistency and difficulty in collecting the data.
To help analyze the impact, SullivanCotter used its proprietary database consisting of individual CPT code volumes and modifiers for approximately 3,000 APPs across 45 different specialties. Two sets of wRVU productivity benchmarks were calculated for comparison. One is based on the pre-2021 wRVU values, and one is based on the 2021 wRVU values. By keeping volumes and distribution consistent, the resulting change in wRVU productivity is due entirely to the E&M wRVU adjustments.
Summary findings indicate that of the 45 specialties reviewed, the average change for all specialties due to the E&M adjustments is 14.6%. As shown in Table 3 below, nearly half (44.4%) of wRVU benchmarks increased between 6% and 17%. An additional 44.4% of specialties were impacted by changes greater than 17%. Only two specialties had changes of less than 1%.
Table 3: Overall APP Specialty Impact of 2021 E&M Changes
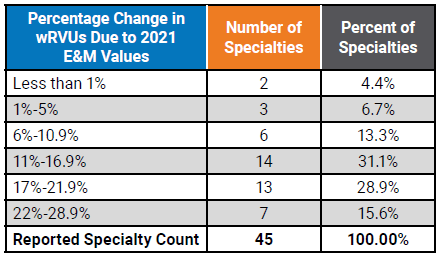
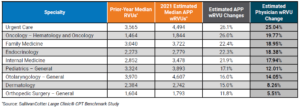
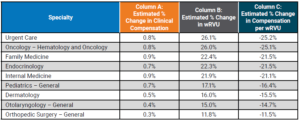
Table 4 below shows a representative sample of the resulting impact at the specialty level. This represents a significant change to wRVU benchmarks in many specialties and will be important for organizations to understand the implications to APP compensation payouts and affordability in all of the various specialties and care teams. Comparing the estimated wRVU changes for APPs and physicians in the same specialty shows general alignment in the medical and primary care specialties with a greater impact on the APPs in surgical specialties due to the higher utilization of E&M visits by APPs compared to physicians.4
Table 4: Median wRVU Impact of 2021 E&M wRVU Changes
2. How will wRVU changes impact compensation for APPs differently than physicians?
The impact will vary for a few notable reasons.
According to SullivanCotter’s 2020 Advanced Practice Provider Compensation and Pay Practices Survey, only 56% of organizations use wRVU data to adjust APP compensation as compared to greater than 90% for physicians.5,6 Because APP compensation is typically salary-based, APPs are less susceptible to compensation impacts due to the CPT adjustments.
Additionally, nearly half of APPs with an incentive component in their compensation plan have the productivity-based incentive amount capped – which will affect the degree to which compensation will be impacted.5
Finally, in our experience, the market compensation per wRVU rate for APPs is often utilized in a different manner compared with physicians. Physician compensation plans typically directly utilize the market compensation per wRVU benchmark rate as a major incentive to drive compensation. For APPs, whose compensation plans are not as heavily incentivized as physician plans, organizations often just utilize market wRVUs and/or compensation per wRVU rates as a guide. Typically, APP plans allow for more significant guaranteed base salaries. Depending on the methodology used for each, this may limit the impact of any increases in APP compensation due to the changes.
Table 5 below highlights the estimated changes to survey benchmarks. See Column A to find the estimated change in compensation.
Table 5: Estimated Survey Benchmark Changes in Clinical Compensation and wRVUs
If an organization utilizes data on wRVU productivity targets to determine compensation using the pre-2021 survey data while calculating wRVUs using the 2021 wRVU schedule, this will result in higher payouts as APPs on incentive plans will meet or exceed the benchmarks at a much greater rate.
Similarly, if an organization uses the pre-2021 compensation per wRVU survey benchmarks while using the new 2021 values to calculate APP productivity, clinical compensation will increase as a result of the pre-adjusted compensation per wRVU rates.
These compensation change estimates are based only on the recalculations of the E&M wRVUs. This does not estimate other market factors that also drive compensation change. Additional factors include supply and demand, inflation, cost-of-living, changes in productivity and more. As with wRVUs, these factors can also vary significantly by specialty.
3. How will this impact APP compensation?
This depends on the structure of an organization’s existing APP compensation program and the degree of productivity incentive. It may have less of an impact than changes to physician compensation for a number of reasons:
- As noted previously, just over half (56%) of organizations use market wRVU data to adjust APP compensation.5
- Only 35% of organizations reported wRVUs for all APPs within the organization.5
- 42% are not tracking or reporting APP wRVUs at all.5
- 49% of organizations report having incentive plans for APPs with wRVUs being the most common component.5
Organizations incentivizing APPs based on wRVU productivity and utilizing national benchmarks to determine annual salaries and compensation per wRVU rates need to assess and understand how these changes to the benchmarks will impact APP compensation payout levels.
SullivanCotter reviewed several different compensation methodologies to estimate the impact on survey benchmarks. Considering the E&M code changes and assuming no modifications are made to compensation plan methodologies, we estimate the average clinical compensation for all APPs to increase by approximately 0.5%. This is compared to approximately 6% for physician compensation identified in Part I.
For organizations with APPs whose pay is structured more like physician compensation, it will be critical to understand the impact these changes will have on incentive plans – which is likely to be far greater than the average 0.5% suggested in this study.
4. If organizations utilize compensation per wRVU benchmarks for APPs, what should they expect with regard to the 2021 benchmarks?
For any group implementing the 2021 rate into their APP compensation plans, a fundamental understanding of how market benchmarks will change is important. This is especially true in some of the procedural specialties where APPs code a much higher number of E&M visits (compared to physicians who are more focused on the procedural codes). As a result, APPs will often see marked increases in wRVUs. It is important to monitor the unintentional impact on work effort for both APPs and physicians as clinicians adapt to the new weighting of professional encounters.
OTHER FACTORS TO CONSIDER WHEN ANALYZING COMPENSATION IMPACTS
As organizations continue to evaluate the impact of the 2021 Physician Fee Schedule, there are several additional factors to consider. These include:
- Are physician and APP compensation plans, incentive opportunities, and metrics aligned and will changes to one component impact the other?
- For specialties that include paid shift rates, are there additional incentives based on productivity?
- Does the organization pay physicians and APPs for virtual care visits that tie to E&M values? This could result in higher compensation for virtual care.
- Will the changes in CPT valuation for telemedicine be permanent or be adjusted after the end of the pandemic?
- CMS will also be adding G2212 as an add-on code for every 15 additional minutes of visit time. The assumptions and analysis above do not account for the changes in the distribution of E&M coding or increases in wRVUs due to these new codes.
- A wRVU increase does not automatically equate to an equal revenue reimbursement increase.
- CMS also applies an annual budget factor that caps the overall per wRVU reimbursement to avoid a significant increase in CMS payments. This can significantly increase the total percentage of revenue an organization receives that can be paid to physicians and APPs.
Sources:
1CMS Releases 2021 Physician Fee Schedule Rule. AAPA News Central. December 2, 2020. Accessed at: https://www.aapa.org/news-
central/2020/12/cms-releases-2021-physician-fee-schedule-rule/
2Proposed Policy, Payment and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2021. August 3, 2020. Centers for Medicare and Medicaid Services. Accessed at: https://www.cms.gov/newsroom/fact-sheets/proposed-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year-4
3Medicare Telemedicine Health Care Provider Fact Sheet. Centers for Medicare and Medicaid Services Fact Sheet. March 17, 2020. https://www. cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
4SullivanCotter Large Clinic® CPT Benchmark Study
5SullivanCotter 2020 Advanced Practice Provider Compensation and Productivity Survey
6SullivanCotter 2020 Physician Compensation and Productivity Survey
SullivanCotter offers advisory support and technology solutions to help your organization understand and respond to the potential impact of these changes.
To learn more, contact us at 888.739.7039 or info@sullivancotter.com