Pay Equity Analysis: Understanding the Entire Story
Pay Equity Analysis: Understanding the Entire Story
Authored by SullivanCotter’s Michael O’Malley – Principal, Nanci Hibschman – Managing Principal and Not-for-Profit Practice Leader, and Amanda Wethington – Principal
Statistical outcomes do not always tell the whole story, and this is particularly true for studies on pay equity.
A statistical finding of no difference in compensation based on gender or race often prematurely ends further discourse on the matter even when the results seem incorrect and inconsistent with many people’s lived experiences. Somehow, pay equity studies do not always capture the reality of what many people are feeling. While statistical analysis is supposed to reflect the true unseen nature of things, the math seems to fail in the instance of pay equity.
The numbers themselves are not to blame. Rather, pay equity studies can be restrictive in focus. They examine whether or not certain groups are equitably paid assuming all else is equal and groups have the same values on other important variables. But often “all else” is not equal and inequalities may not show up because the analyses presume no relevant differences between the groups being evaluated. Yet, important differences can exist in a number of ways.
SullivanCotter describes three areas where differences may exist, how they avoid detection in standard pay equity assessments, and what further analyses are required to help complete a story only partially told.
Selection Bias
Pay equity analyses are conducted on the organization’s current workforce. However, if members of certain groups leave the organization at differential rates and one of the reasons for this turnover is low wages, then the current workforce does not represent those who may be underpaid. By eliminating a group of low-paid employees, the comparison to the remaining members of the workforce will appear more favorable. To understand if members of certain groups are more apt to self-select out of the organization, studies that examine the incidence of turnover and compensation levels of employees who have left are necessary.
Performance Bias
Pay equity analyses that include performance as a factor will “correct” any differences between groups based on this variable. But that approach begs the important question: Why might groups differ on performance? As it happens, there are a number of well-documented reasons for these differences – and none concern actual ability. For example, women and people of color must perform at higher levels than white males to be seen as performatively equivalent. Additionally, other performance-enhancing opportunities such as access to training, developmental assignments, guided learning projects, and mentorship may not be the same for everyone. The only way to know if this is the case is to see if differences in access to these opportunities exist.
Career Bias
Generally, women and people of color do not occupy as high of rank as white males in organizations and, on average, receive lower compensation. It is not simply that there are fewer women and people of color in leadership positions, but that they are disproportionately absent. Again, the pay equity analyses will calibrate for hierarchical disparities when comparatively examining compensation. But what happens to women and people of color during their career trajectories? Do they make slower career progress or stall at certain organizational levels? Again, the literature is replete with studies on career-family imbalances and the sacrifices working women, for example, must make to sustain the viability of both their home and work lives. Only further analyses can say if there is a price that certain groups must pay.
If your organization is looking to conduct a meaningful pay equity analysis that gets to the root of the actual issue rather than remaining content with what is being outwardly projected, you’ll need to take the time to understand the entire story and assess whether or not the pay equity that may seem so apparent is truly equitable or not.
DOWNLOAD PDF
Need assistance assessing pay equity with your organization?
With years of industry experience and a deeply knowledgable team of compensation experts, SullivanCotter is uniquely positioned to address your pay equity needs.
RELATED ARTICLES
RELATED SERVICES
PRESS RELEASE | Pay Equity Expert Mike O'Malley Joins SullivanCotter
Pay equity is an important prerequisite for fostering a fully engaged workforce
Chicago, IL | May 24, 2022
SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, is pleased to announce the addition of prominent social psychologist and research-driven consultant Mike O’Malley as a Principal in the firm’s Employee Workforce Practice.
As a leader in his field, Mike has spent more than 30 years consulting and educating boards and senior executives on a myriad of human capital matters such as leadership development, compensation, succession planning, change management and more. He is also a widely published author specializing in leadership excellence and organizational design and leverages years of experience in his research-based approach with clients.
In his role at SullivanCotter, Mike partners with health care and other not-for-profit organizations to develop data-driven solutions that enhance performance and help achieve strategic goals. He assists in overseeing the firm’s pay equity analyses and advisory services. With a focus on both performance and equity, he leads critical compensation and benefits redesign initiatives to provide a more holistic and integrated approach to total rewards.
“As a fundamental element of inclusion and belonging initiatives, pay equity is an important prerequisite for fostering a fully engaged workforce. These services are a pivotal component of our commitment to helping clients build stronger organizations that are representative, inclusive, and fair – and Mike’s longstanding expertise in this area will help to support these goals”, said Ted Chien, President and Chief Executive Officer, SullivanCotter.
Previously, Mike held leadership positions in a number of prominent global consulting firms. He currently serves as a Lecturer at the Yale University School of Medicine, where he conducts research and consults on statistics and a broad range of human resources topics.
In addition to having his expertise recognized by major media outlets such as CNBC, CBS and Fox, Mike has also been the keynote speaker at national and international events hosted by the United States Department of the Interior, the Financial Times, the London School of Economics and Political Science, and the Henry Jackson Society.
About SullivanCotter
SullivanCotter partners with healthcare and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology products to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON PR NEWSWIRE
PODCAST | Submitting Split/Shared Visits for Reimbursement
Zach Hartsell, Principal – APP Workforce Practice – featured in BESLER’s Hospital Finance Podcast to discuss changes to split/shared visit attribution
Listen to podcast >
Every year, the Centers for Medicare & Medicaid Services incorporate changes in policy, regulations, and requirements for billing under the Medicare Physician Fee Schedule (PFS). These changes are often adopted by commercial payers.
On November 2, 2021, CMS released the final rule for the 2022 PFS. The final rule went into effect on January 1, 2022, and includes some important considerations related to the conditions for submitting split-shared visits for reimbursement.
These changes have the potential to alter the existing workflow of physicians and advanced practice providers related to billing split-shared encounters.
To help explain the impact of these changes, this episode includes:
- The definition of a split/shared visit
- Insight into the 2022 changes as well as those coming in 2023
- Explanation of specific activities that CMS has identified
- Case-based examples
Looking for additional insight on the changes to the Physician Fee Schedule regarding Split/Shared Visits?
We’ve recently published some content that may be of interest to you.
ARTICLE
Physician Fee Schedule: Understanding Changes to Split/Shared Visits
INFOGRAPHIC
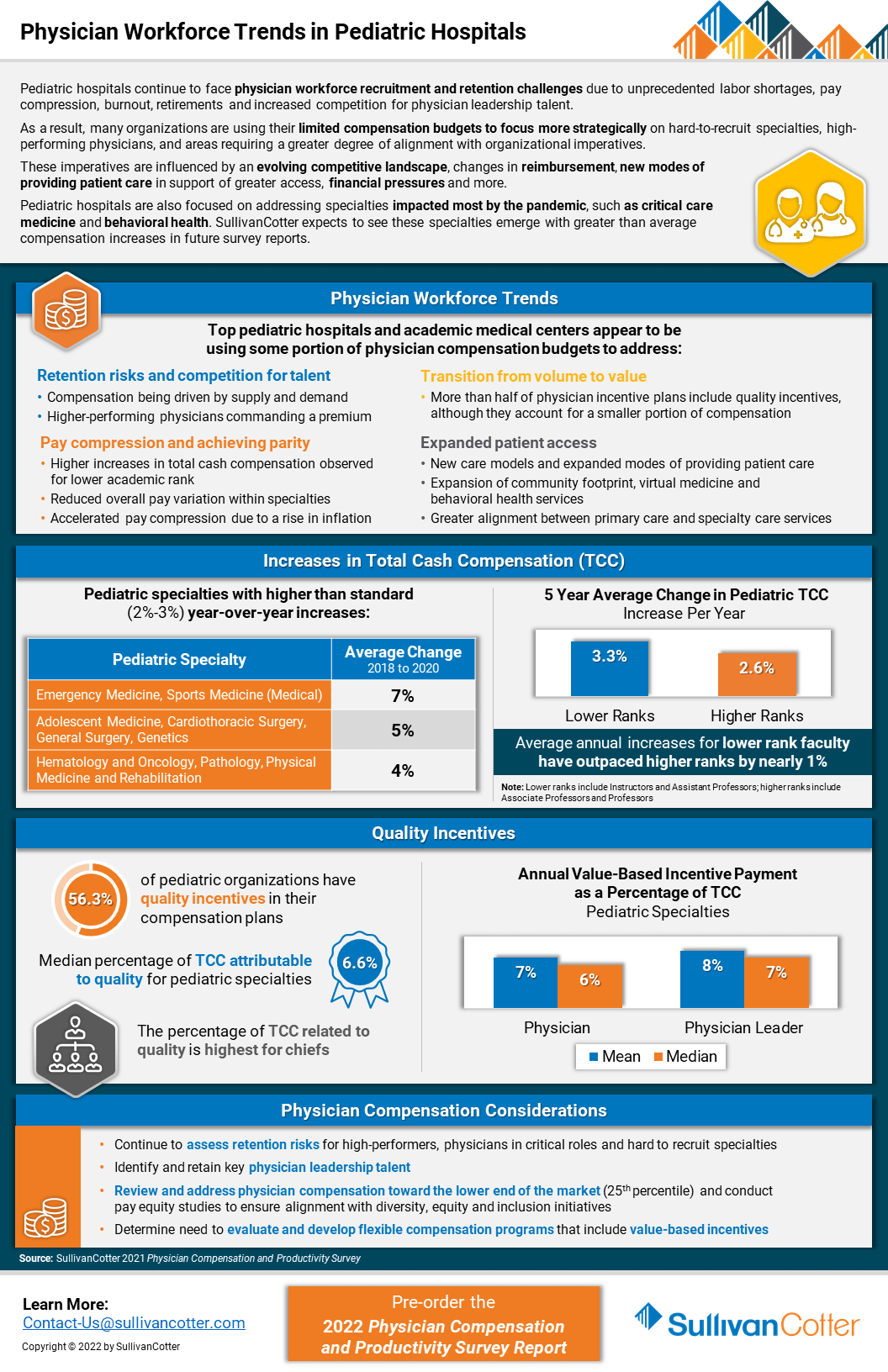
INFOGRAPHIC | Physician Workforce Trends in Pediatric Hospitals
Pediatric hospitals continue to face physician workforce recruitment and retention challenges
Due to unprecedented labor shortages, pay compression, burnout, retirements and increased competition for physician leadership talent, pediatric organizations are experiencing a number of challenges related to recruiting and retaining the right talent.
As a result, many organizations are using their limited compensation budgets to focus more strategically on hard-to-recruit specialties, high-performing physicians, and areas requiring a greater degree of alignment with organizational imperatives.
These imperatives are influenced by an evolving competitive landscape, changes in reimbursement, new modes of providing patient care in support of greater access, financial pressures and more.
Pediatric hospitals are also focused on addressing specialties impacted most by the pandemic, such as critical care medicine and behavioral health. SullivanCotter expects to see these specialties emerge with greater than average compensation increases in future survey reports.
VIEW INFOGRAPHIC
PODCAST | Executive Compensation Committee
Priorities and Trends for the Executive Compensation Committee
Episode 1 >
Episode 2 >
In a rapidly evolving health care environment, oversight of executive compensation, recruitment and retention remains a critical responsibility of the board of directors. These decisions are complex, highly regulated and require heightened executive compensation committee engagement and specialized expertise.
In this two-part edition of the Governing Health Podcast Series, SullivanCotter's Tim Cotter, Managing Director, joins McDermott Will & Emery's Michael Peregrine to discuss emerging trends and practices in health care executive compensation.
These episodes include insight into:
- The current state of salaries, increase budgets, incentive awards and more
- Emerging compensation practices
- Effective retention and transition strategies
- The evolution of annual and long-term incentive plans
- Executive and director co-investment arrangements
- For-profit compatibility data
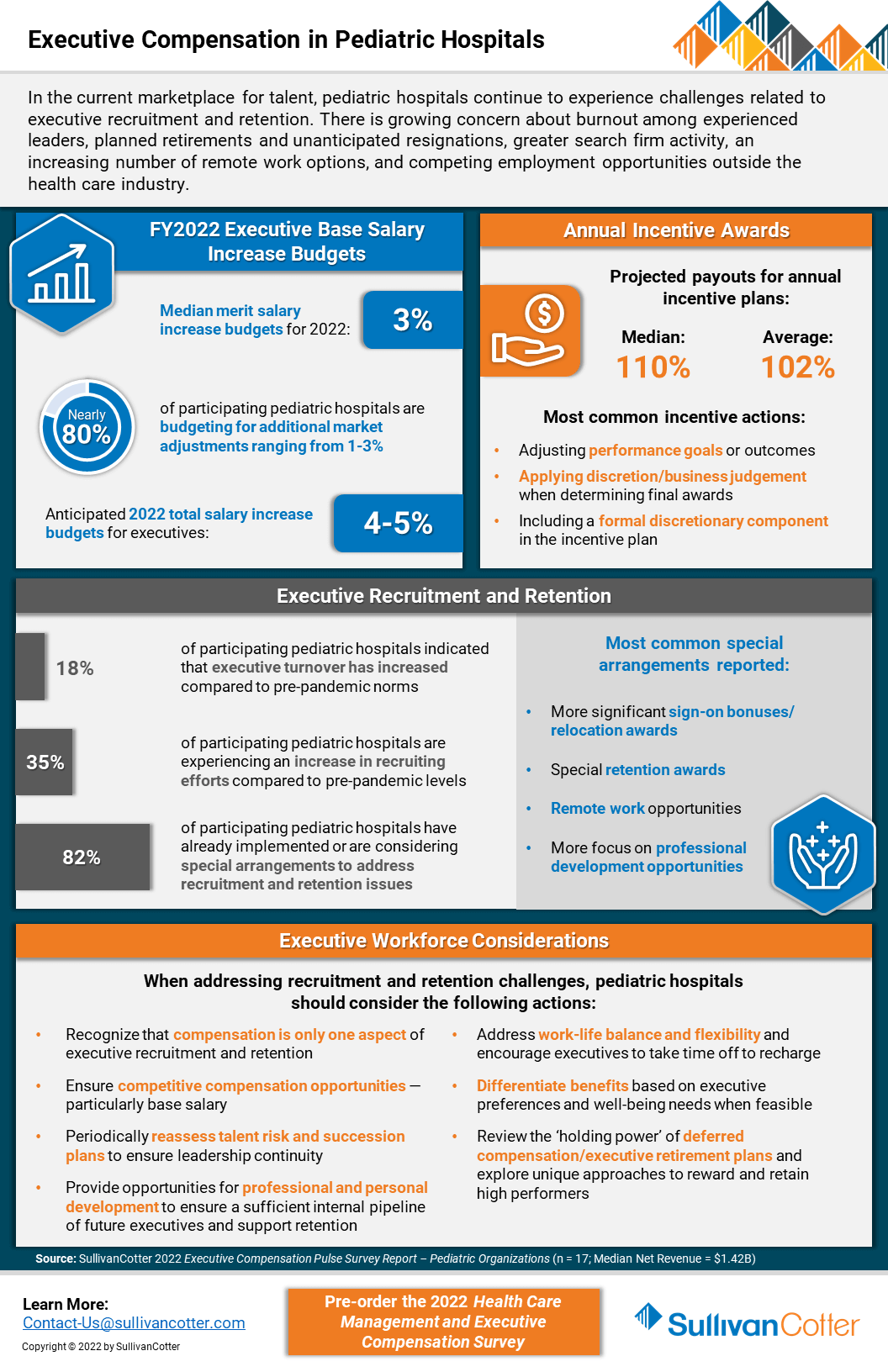
INFOGRAPHIC | Executive Compensation in Pediatric Hospitals
SullivanCotter addresses executive compensation in pediatric hospitals via a recent pulse survey
In the current marketplace for talent, executive compensation in pediatric hospitals is growing increasingly complex as recruitment and retention challenges mount. Organizations remain concerned about burnout among experienced leaders, planned and unanticipated resignations, greater search firm activity, employment opportunities outside the healthcare industry, and remote work presenting more non-traditional employment opportunities.
SullivanCotter recently conducted a pulse survey to help pediatric hospitals understand how their peers are addressing 2022 executive salary increase budgets and incentive awards for FY2021 performance.
It also highlights other actions these organizations are taking to support executive recruitment and retention.
VIEW INFOGRAPHIC
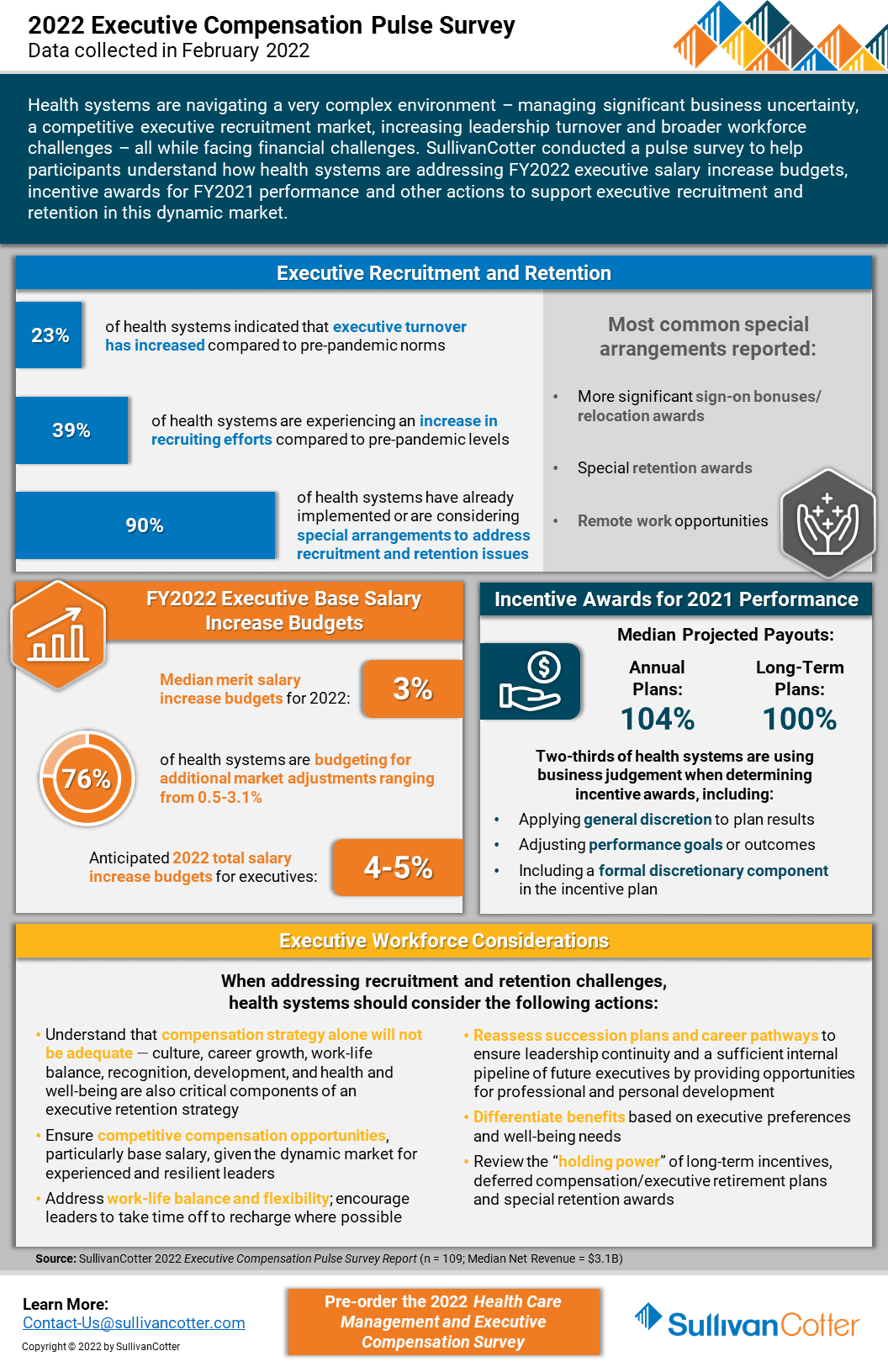
INFOGRAPHIC | 2022 Executive Compensation Pulse Survey
SullivanCotter’s recent executive compensation pulse survey provides insight into how healthcare organizations are addressing recruitment and retention challenges in an increasingly dynamic marketplace
Health systems are growing increasingly concerned about burnout among experienced leaders, planned retirements and unanticipated resignations, greater search firm activity and employment opportunities outside the healthcare industry, as well as remote work presenting more non-traditional employment opportunities.
Considering these concerns, SullivanCotter conducted an executive compensation pulse survey to help participants understand how health systems are addressing FY2022 salary increase budgets and incentive awards for FY2021 performance.
It also highlights other actions systems are taking to support executive recruitment and retention in this dynamic market.
VIEW INFOGRAPHIC
PRESS RELEASE | Wayne Hartley Joins SullivanCotter to Help Expand Physician Workforce Advisory Services
Longstanding knowledge in health care operations, finance and human resources
Chicago, IL | March 29, 2022
SullivanCotter, the nation's leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, is pleased to welcome back Wayne Hartley as a Principal in the firm's Physician Workforce Practice.
Wayne is an accomplished senior consulting leader with a distinguished history of managing high-quality medical operations and utilizes more than 20 years of direct healthcare industry experience in his work with clients. With longstanding knowledge in healthcare operations, finance and human resources, Wayne specializes in helping organizations to strengthen physician compensation program strategy, regulatory compliance and value-based outcomes.
"As healthcare organizations look for innovative ways to stay ahead of the curve in an ever-changing marketplace, our aim is to leverage a diverse and growing panel of expertise from the industry's best and brightest consultants. We're thrilled to welcome Wayne back to SullivanCotter and, with his unique skillset and insight, look forward to learning from his extensive clinical and operational leadership experience, building strategic partnerships with new and existing clients, and expanding the firm's clinical workforce advisory services," said Mark Ryberg, Physician Workforce Practice Leader, SullivanCotter.
In his new role with SullivanCotter, Wayne will work with clients to lead physician compensation design projects and develop models to support organization-wide goals as they relate to patient access, panel size, productivity, quality and more. Additionally, he will advise organizations on the fair market value and commercial reasonableness of physician transactions to enhance compliance and mitigate risk, liaise with boards and physician leaders on high-value business strategies, and introduce new methodologies to assess and improve health system readiness for risk-based reimbursement.
Wayne also serves on the firm's Large Clinic™ Group Growth Team in which he helps to direct strategy and member engagement for the 45-year-old independent affinity group comprised of the largest medical organizations in the U.S.
Prior to joining the firm, Wayne previously served in a variety of leadership positions for a number of nationally-recognized consulting firms. He also has a wealth of clinical and operational experience from his time at two of the largest health systems in Minneapolis.
About SullivanCotter
SullivanCotter partners with healthcare and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology products to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON PR NEWSWIRE
PRESS RELEASE | Enhancing PPMT™ User Experience for Physicians and APPs
Identifying opportunities to educate and engage the clinical workforce
Chicago, IL | March 23, 2022
SullivanCotter, the nation's leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, announces new functionality for its growing Provider Performance Management Technology™ (PPMT™) platform that enhances ease of access and usability for physicians and advanced practice providers (APPs). PPMT™ is an industry-first, cloud-based product that engages the clinical workforce and informs leaders through transparent performance-based compensation administration, contract management, and analytical and reporting capabilities.
New functionality includes valuable upgrades to the PPMT™ portal – allowing physicians and APPs one-click access to view key performance indicators via mobile or desktop. This provides physicians and APPs with a quicker line of sight into current performance and productivity results and enhances their ability to track progress against goals on their personal landing page. PPMT's more robust reporting capabilities are also still available for clinicians who are looking to dive deeper into detailed productivity, performance, and compensation results.
The focus on physician and APP engagement is further enhanced with the addition of self-service utilization reporting for compensation administrators. Enabling administrators to easily see which physicians and APPs have been utilizing PPMT™ and what reports have been accessed helps them to identify opportunities to engage the clinical workforce. "Administrators, leaders and managers are often having conversations with individual clinicians about their compensation and these reports help them to go into these meetings better prepared with opportunities to engage and educate their colleagues," said Shelly Slowiak, Director of Product Support - PPMT™, SullivanCotter.
Designed to address a spectrum of physician, leadership and other key stakeholder needs, PPMT™ combines years of healthcare compensation insight and expertise with an intuitive and automated technology platform to help drive performance and support the transition from volume- to value-based care.
"The needs of the health care organizations we serve are dynamic and ever-changing – especially in a marketplace that has grown increasingly complex in the past two years. SullivanCotter remains dedicated to continually enhancing our technology products to drive greater value for clients by understanding these needs and evolving alongside them," said David Schwietz, Chief Information Officer, SullivanCotter.
For more information on these enhancements or our entire suite of Provider Performance Management Technology™, visit www.sullivancotter.com/PPMT or contact us at 888.739.7039.
About SullivanCotter
SullivanCotter partners with health care and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology products to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON PR NEWSWIRE
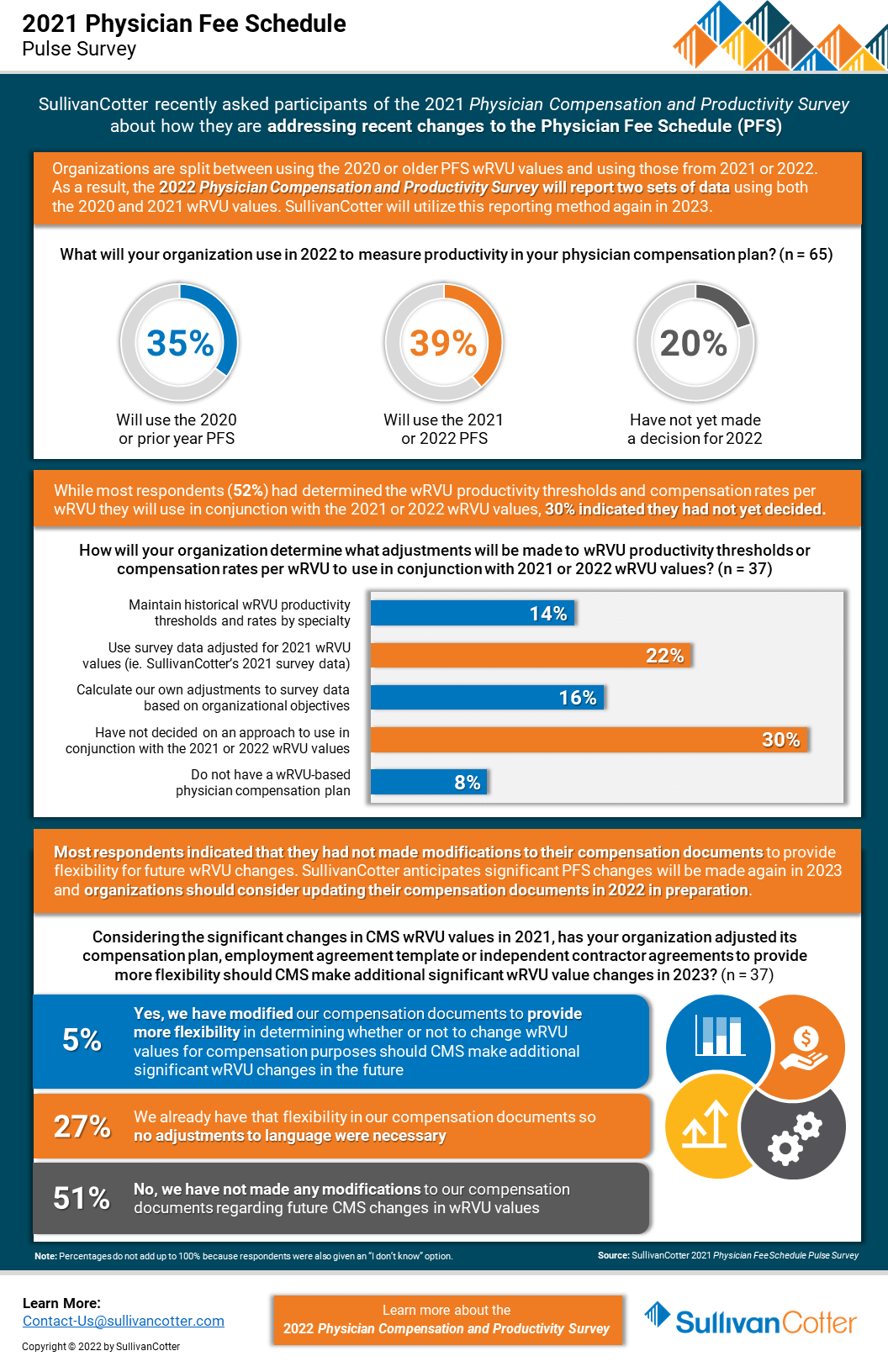
INFOGRAPHIC | Pulse Survey Results: 2021 Physician Fee Schedule Changes
How are health care organizations addressing the 2021 Physician Fee Schedule changes?
Following its annual review of the American Medical Association’s Relative Value System Update Committee’s recommendations, the Centers for Medicare and Medicaid Services (CMS) finalized proposed changes to the 2021 Physician Fee Schedule and has significantly overhauled the Evaluation and Management (E&M) code documentation requirements, time-effort recognition, and wRVU values for new and established patient office visits. These changes were effective as of January 1, 2021.
As organizations look to understand the impact of these changes on reported physician productivity levels, it is also important to assess the effect it will have on physician compensation arrangements, fair market value and commercial reasonableness considerations, financial sustainability and national survey benchmarks.
SullivanCotter recently conducted a pulse survey for participants in the 2021 Physician Compensation and Productivity Survey to assess how organizations are addressing these changes. View highlights from the results – including insight into expected adjustments to work RVU productivity thresholds and compensation rates per work RVU.
VIEW INFOGRAPHIC
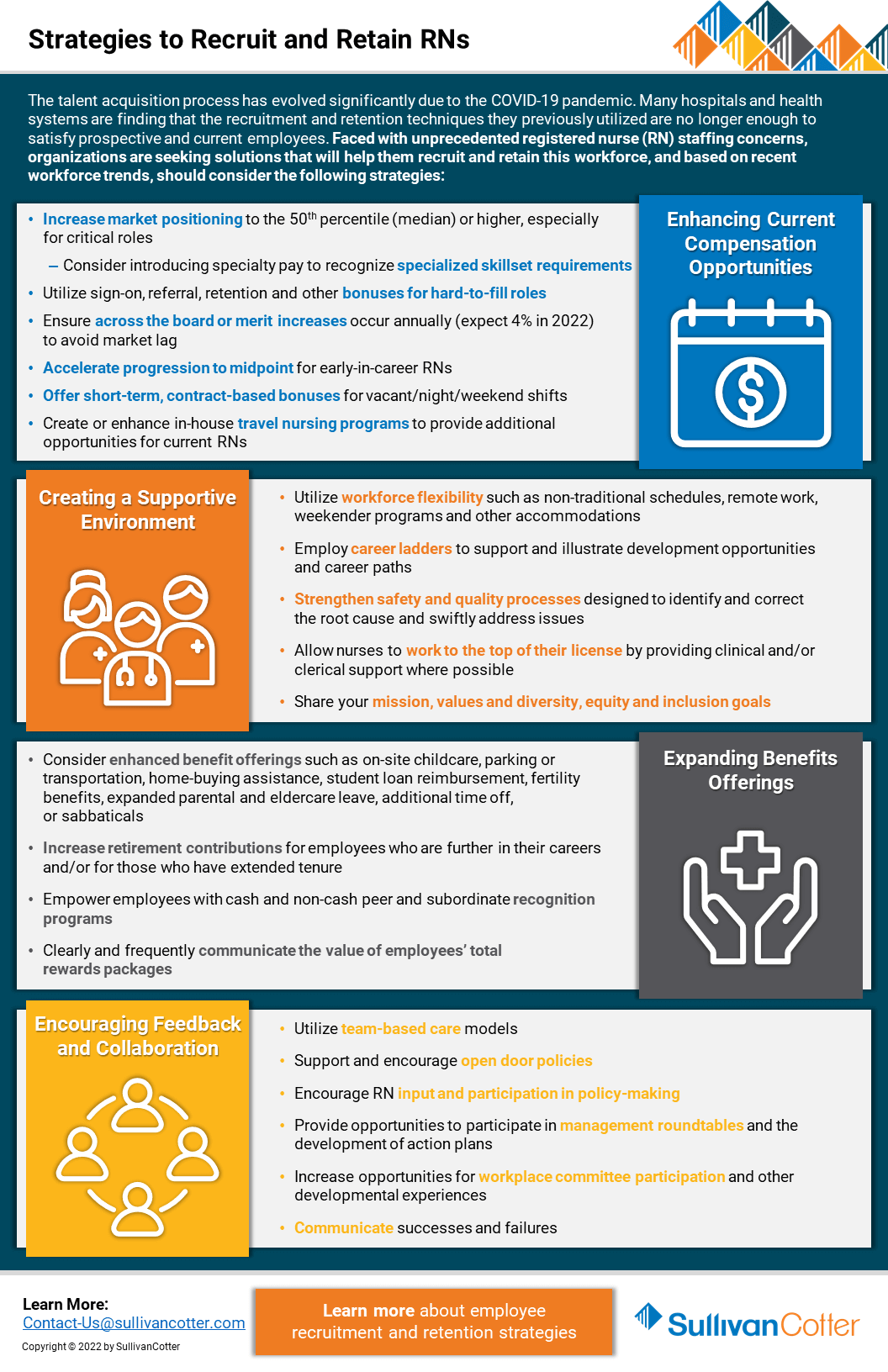
Registered Nurses | Strategies to Recruit and Retain
Looking for better strategies to recruit and retain registered nurses?
The talent acquisition process has evolved significantly due to the COVID-19 pandemic. Many hospitals and health systems are finding that the recruitment and retention techniques they previously utilized are no longer enough to satisfy prospective and current employees. Faced with unprecedented staffing concerns regarding registered nurses (RN), organizations are seeking solutions that will help them recruit and retain this workforce.
Based on recent workforce trends, hospitals and health systems should consider the following strategies:
Enhancing Current Compensation Strategies
- Increase market positioning to the 50th percentile (median) or higher, especially for critical roles
- Consider introducing specialty pay to recognize specialized skillset requirements
- Utilize sign-on, referral, retention and other bonuses for hard-to-fill roles
- Ensure across-the-board or merit increases occur annually (expect 4% in 2022) to avoid market lag
- Accelerate progression to midpoint for early-in-career RNs
- Offer short-term, contract-based bonuses for vacant/night/weekend shifts
- Create or enhance in-house travel nursing programs to provide additional opportunities for current RNs
Creating a Supportive Environment
- Utilize workforce flexibility such as non-traditional schedules, remote work, weekender programs and other accommodations
- Employ career ladders to support and illustrate development opportunities and career paths
- Strengthen safety and quality processes designed to identify and correct the root cause and swiftly address issues
- Allow nurses to work to the top of their license by providing clinical and/or clerical support where possible
- Share your mission, values, and inclusion and belonging goals
Expanding Benefits Offerings
- Consider enhanced benefit offerings such as on-site childcare, parking or transportation, home-buying assistance, student loan reimbursement, fertility
benefits, expanded parental and eldercare leave, additional time off, or sabbaticals - Increase retirement contributions for employees who are further in their careers and/or for those who have extended tenure
- Empower employees with cash and non-cash peer and subordinate recognition programs
- Clearly and frequently communicate the value of employees’ total rewards packages
Encouraging Feedback and Collaboration
- Utilize team-based care models
- Support and encourage open-door policies
- Encourage RN input and participation in policy-making
- Provide opportunities to participate in management roundtables and the development of action plans
- Increase opportunities for workplace committee participation and other developmental experiences
- Communicate successes and failures
Looking for additional workforce insights and data?
Contact us to learn more about employee recruitment and retention strategies
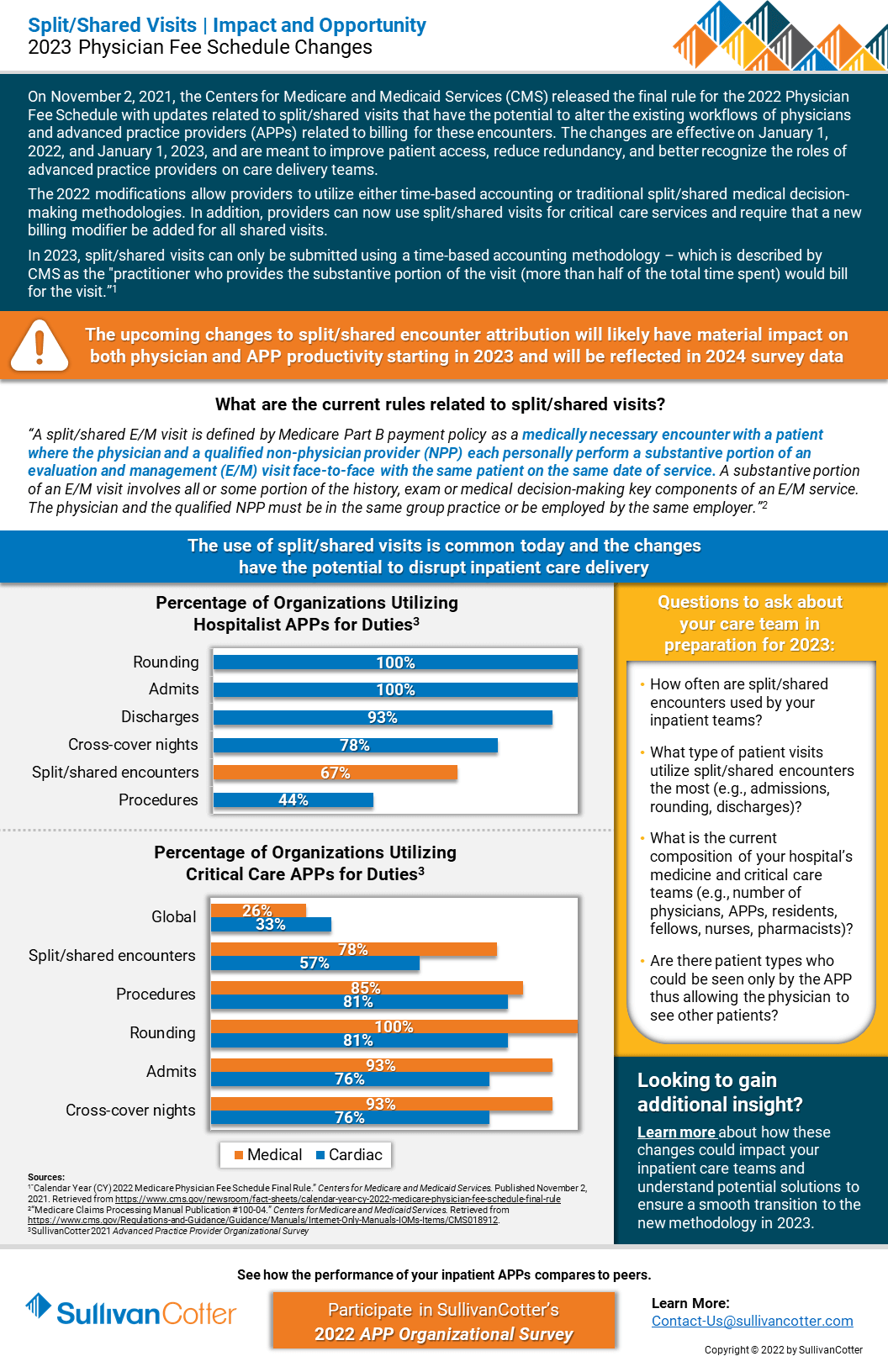
INFOGRAPHIC | Split/Shared Visits
Split/Shared Visits: Understanding the impact and opportunity of the 2023 Physician Fee Schedule Changes
RELATED CONTENT
ARTICLE | 2022 Physician Fee Schedule Changes
On November 2, 2021, the Centers for Medicare and Medicaid Services (CMS) released the final rule for the 2022 Physician Fee Schedule with updates related to split/shared visits that have the potential to alter the existing workflows of physicians and advanced practice providers (APPs) related to billing for these encounters. The changes are effective on January 1, 2022, and January 1, 2023, and are meant to improve patient access, reduce redundancy, and better recognize the roles of advanced practice providers on care delivery teams.
The 2022 modifications allow providers to utilize either time-based accounting or traditional split/shared medical decision-making methodologies. In addition, providers can now use these visits for critical care services and require that a new billing modifier be added for all shared visits.
In 2023, split/shared visits can only be submitted using a time-based accounting methodology – which is described by as the “practitioner who provides the substantive portion of the visit (more than half of the total time spent) would bill or the visit.”
Learn more about the current rules related to split/shared visits.
VIEW INFOGRAPHIC
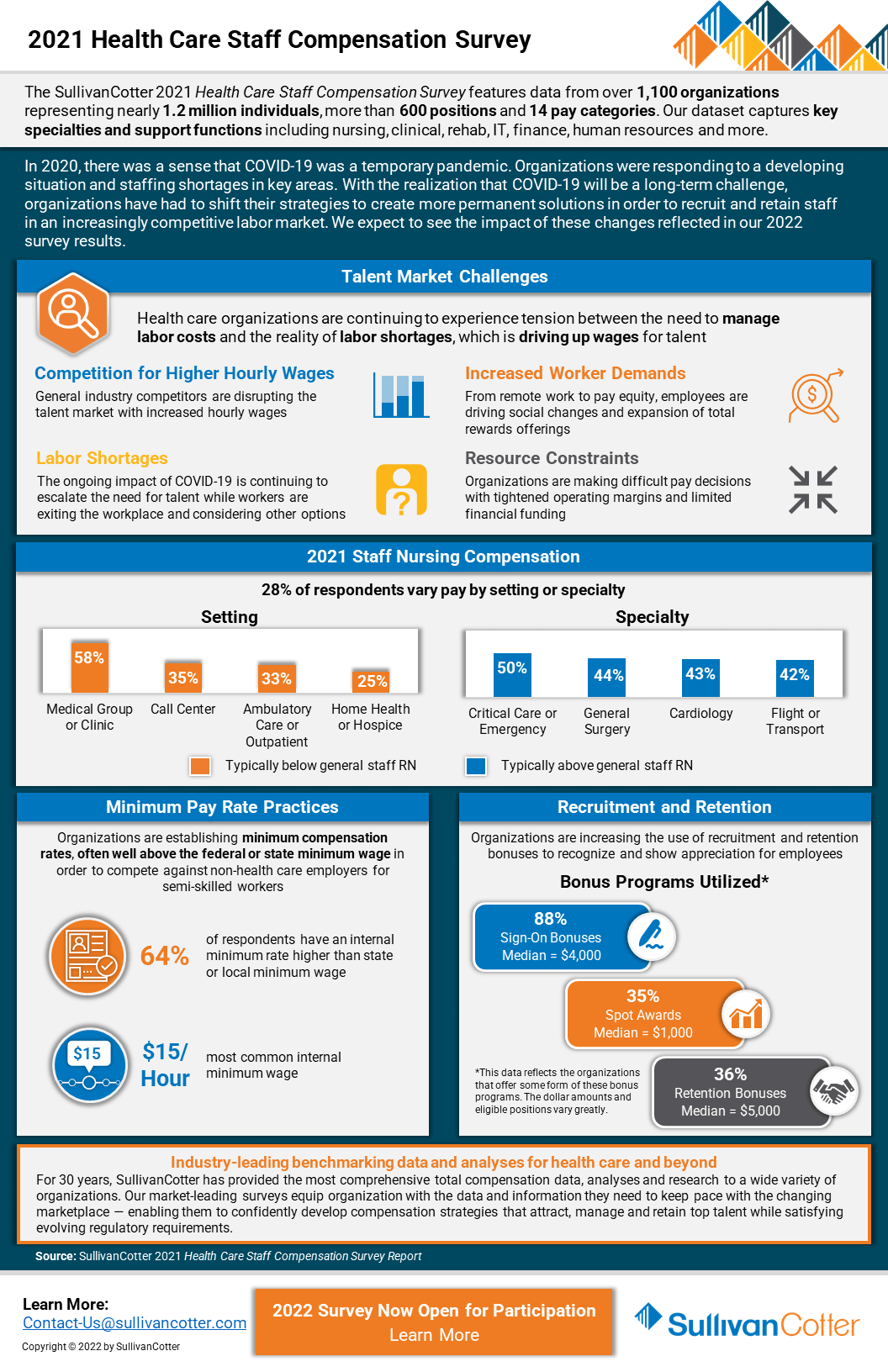
INFOGRAPHIC | 2021 Health Care Staff Compensation Survey
Hospitals and health systems continue to experience tension between the need to manage labor costs and healthcare staff compensation with the reality of employee workforce shortages
In 2020, there was a sense that COVID-19 was a temporary pandemic. Organizations were responding to a developing situation and dealing with staffing shortages in key areas.
Results from SullivanCotter’s 2021 Health Care Staff Compensation Survey help to shed some light on the impact of the pandemic on the industry’s employee workforce. Featuring data from over 1,100 organizations representing nearly 1.2 million individuals, more than 600 positions and 14 pay categories, this dataset provides insight into key specialties and support functions including nursing, clinical, rehab, IT, finance, human resources and more.
With the realization that COVID-19 will be a long-term challenge, organizations have had to shift their strategies to create more permanent solutions in order to recruit and retain staff in an increasingly competitive labor market. We expect to see the impact of these changes reflected in our 2022 survey results.
The 2022 survey is now open! Submit data to gain access to exclusive participant benefits.
DOWNLOAD INFOGRAPHIC
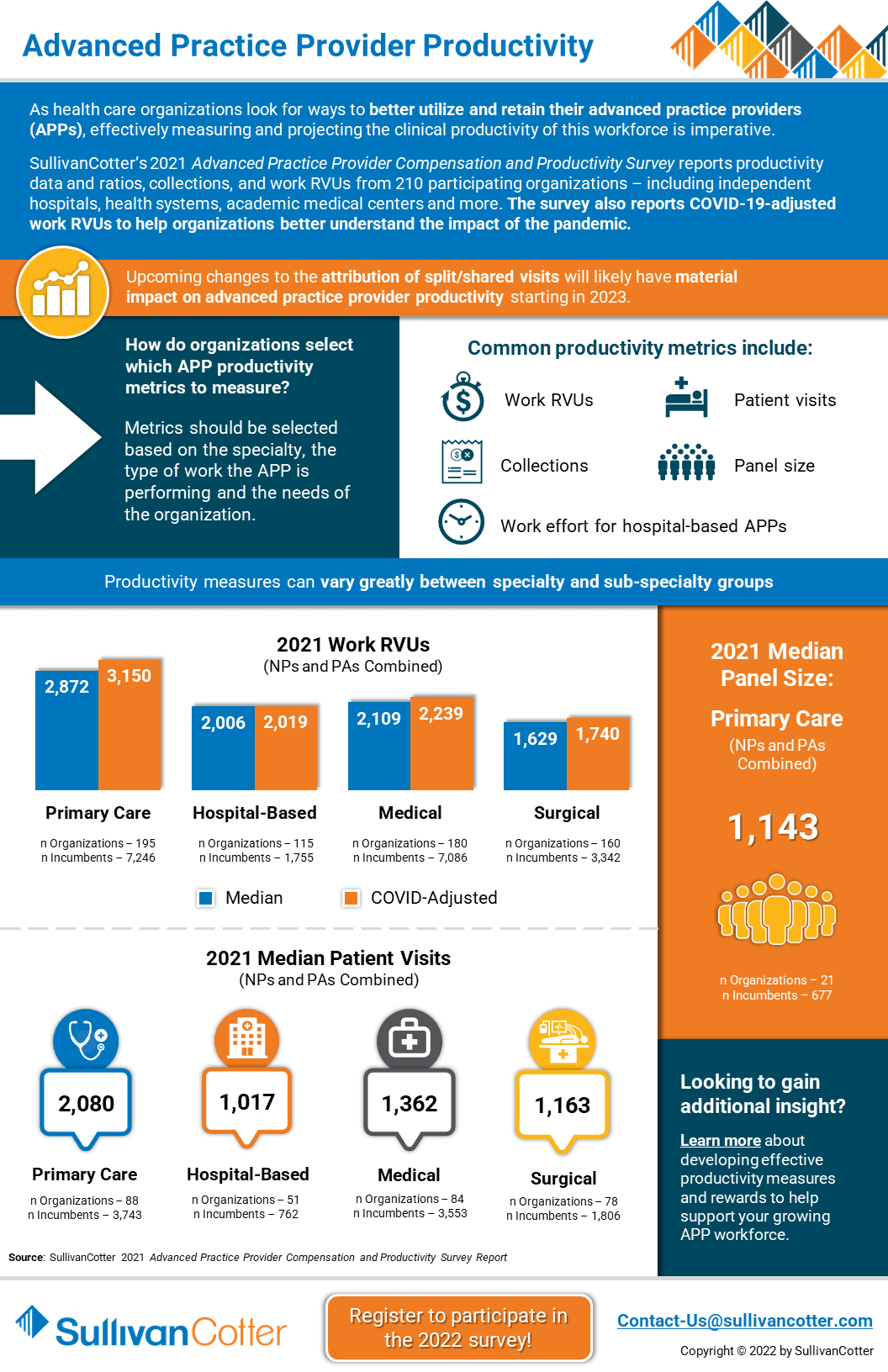
INFOGRAPHIC | Advanced Practice Provider Productivity
How do healthcare organizations select which APP productivity metrics to measure?
As healthcare organizations look for ways to better utilize and retain their clinical workforce, effectively measuring and projecting advanced practice provider productivity is imperative.
SullivanCotter’s 2021 Advanced Practice Provider Compensation and Productivity Survey reports productivity data and ratios, collections, and work RVUs from 210 participating organizations – including independent hospitals, health systems, academic medical centers and more. The survey also reports COVID-19-adjusted work RVUs to help organizations better understand the impact of the pandemic.
The 2022 survey is now open! Submit data to gain access to exclusive participant benefits.
Looking to gain additional insight?
Learn more about developing effective productivity measures and rewards to help support your growing APP workforce.
DOWNLOAD INFOGRAPHIC
E-Book | Key Agenda Items for Health Care Board Committees
Supporting health care board committee effectiveness in a changing environment
ACCESS E-BOOK
SullivanCotter has contributed two chapters to the third edition of the comprehensive e-book from McDermott Will & Emery entitled Key Agenda Items for Board Committees: Supporting Committee Effectiveness in a Changing Environment.
> Trends and Priorities for the Human Capital Committee
Authors: Tim Cotter, Managing Director - Kathy Hastings, Executive Workforce Practice Leader - Cathy Loose, Employee Workforce Practice Leader
Is your organization equipped to address ongoing industry challenges in 2022 and beyond? COVID-19 has not only accelerated dramatic shifts within health care, it also has become a catalyst for change in workforce strategies. Identifying emerging trends and practices and understanding their impact is important for the human capital committee to consider as it plans for the upcoming year.
> 10 Questions for the Compensation Committee
Authors: Tim Cotter, Managing Director - Bruce Greenblatt, Managing Principal
What important items should the Compensation Committee be considering as it plans for 2022 and beyond? SullivanCotter addresses important committee priorities, compensation-related matters such as executive salary adjustments and incentive programs, critical inclusion and belonging initiatives, and more.
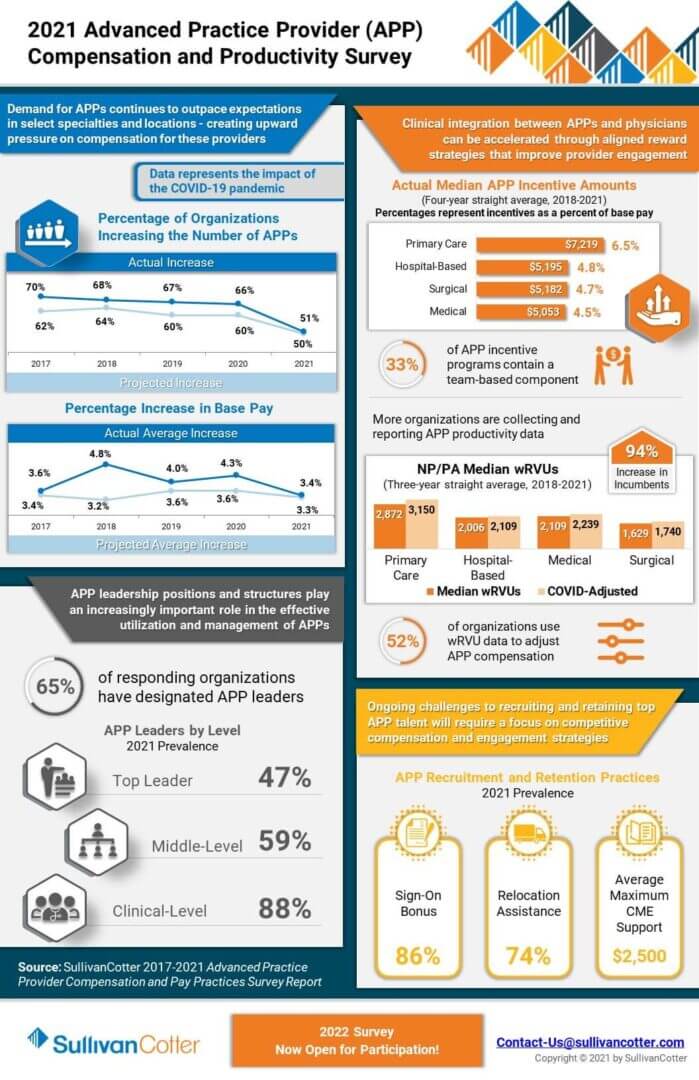
INFOGRAPHIC | 2021 Advanced Practice Provider Compensation and Productivity Survey
Market-leading survey data to help manage the growing APP workforce
As healthcare organizations nationwide continue to increase the size of their advanced practice provider workforce, the market’s interest in data-driven intelligence to help recruit, retain, and engage this critical provider group is growing.
View highlights from SullivanCotter’s 2021 APP Compensation and Productivity Survey – featuring data on more than 92,000 thousand individual APPs (nurse practitioners, physician assistants, certified registered nurse anesthetists, certified anesthesiologist assistants and certified nurse midwives) and nearly 2,200 APP leaders.
The survey collects and reports important advanced practice provider benchmarking information as it relates to utilization, productivity, compensation, pay practices as well as addressing important issues such as APP turnover and vacancy rates. Additionally, this year’s results contain the first set of benchmark data following the onset of COVID-19 and represent an important resource for organizations needing pre and post-pandemic reference points.
The 2022 survey is now open! Submit data to gain access to exclusive participant benefits.
DOWNLOAD INFOGRAPHIC
PRESS RELEASE | Aimee Greeter Joins Physician Workforce Practice
Leading pay and career equity initiatives with organizations looking to improve fairness, transparency and advancement
Chicago, IL | January 25, 2022
SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, is pleased to announce the addition of Aimee Greeter, Principal, to the firm’s growing Physician Workforce Practice.
For nearly 15 years, Aimee has served as a trusted advisor to a variety of healthcare provider organizations nationwide. As the industry continues to undergo significant change, Aimee works with physician groups and health systems of all sizes to develop competitive compensation and rewards strategies focused on supporting pay equity and enhancing physician engagement.
“In the wake of a COVID-19 resurgence, recent changes to the Physician Fee Schedule, and a looming provider shortage, hospitals and health systems are dealing with a myriad of challenging present-day obstacles,” said Mark Ryberg, Physician Workforce Practice Leader, SullivanCotter. “Aimee’s deep-seated industry knowledge and strategic insight reinforces our ability to provide clients with the guidance needed to develop innovative solutions to complex issues as they plan for 2022 and beyond.”
Aimee specializes in helping organizations assess, develop and implement pay and career equity initiatives and consults with employers on ways to improve fairness, transparency and advancement for all people regardless of their gender identity, race and ethnic background. She also works closely with clients to optimize physician and advanced practice provider alignment and affiliation activities to support quality care outcomes, cost efficiencies, integrated care team delivery and patient-centered operations.
Aimee has additional experience in conducting clinical service line reviews, providing advisory support on mergers and acquisitions, and facilitating boards and executive leaders in strategic planning and growth initiatives related to market sustainability, care delivery transformation and business model evolution.
Before joining SullivanCotter, Aimee held senior leadership roles at a boutique health care consulting group.
Aimee is the author of the recently published book Effective Crisis Leadership in Healthcare: Lessons Learned from a Pandemic and is a popular national speaker on topics of crisis leadership, health care transactions and provider engagement. She is also a Fellow in the American College of Healthcare Executives and holds a Lean Six Sigma Yellow Belt.
READ ON NEWSDIRECT
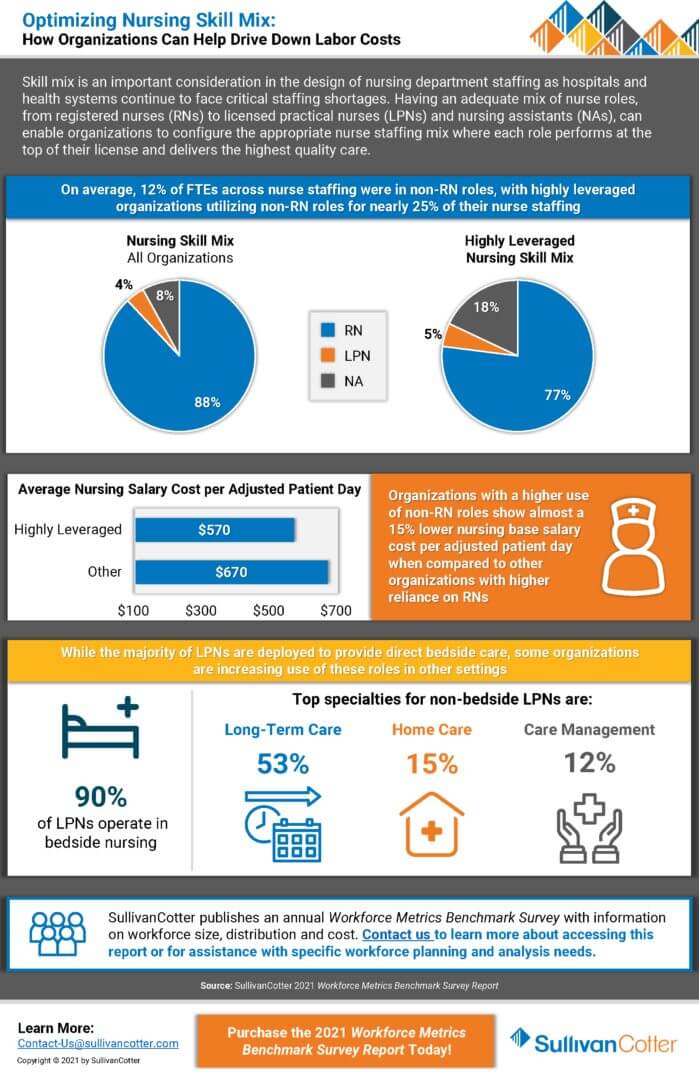
INFOGRAPHIC | Optimizing Nursing Skill Mix
How Organizations Can Help Drive Down Labor Costs
Nursing skill mix is an important consideration in the design of nursing department staffing as hospitals and health systems continue to face critical staffing shortages. Having an adequate mix of nurse roles, from registered nurses (RNs) to licensed practical nurses (LPNs) and nursing assistants (NAs), can enable organizations to configure the appropriate nurse staffing mix where each role performs at the top of their license and delivers the highest quality care.
Looking for additional workforce insights and data?
PRESS RELEASE | SullivanCotter Releases Annual Workforce Metrics Benchmark Survey Results
SullivanCotter Releases Annual Workforce Metrics Benchmark Survey Results and Offers Insight Into Health Care Workforce Structure
Chicago, IL | December 08, 2021 01:26 PM Eastern Standard Time
SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and technology and data products for the healthcare industry and not-for-profit sector, recently released results from its 2021 Workforce Metrics Benchmark Survey.
The survey contains benchmark data on 10 staff level job families, including Ancillary Services, Care Management, Emergency Medical Services, Facilities Services, Financial Services, Human Resources, Information Technology, Legal and Compliance Services, Nursing, and Technical Medical Support. “Insights from this survey will arm health care organizations with essential information on how the composition and cost of their workforce compares to the market,” said James Roth, Managing Principal, SullivanCotter.
“Healthcare organizations face unprecedented pressure as disruptions in patient volume, reductions in employer-sponsored insurance, labor shortages and rising expenses all remain key challenges. As these organizations look for better ways to optimize care delivery and improve performance, effectively managing the size, shape and architecture of the workforce is critical. By gaining an understanding of how your organization compares to industry benchmarks, you can better support operational restructuring decisions that help manage labor expenses, recognize acquisition-related cost saving opportunities, identify retirement risks, and uncover gaps in meeting your diversity objectives,” said Roth.
Increased Attention on Workforce Architecture
Understanding the drivers of workforce cost requires a multi-dimensional analysis that must take into consideration the interaction between three factors – the overall size of the workforce, the distribution of the workforce across career levels and the job level pay position relative to your target market.
“The tension between responding to a compressed labor market and rising labor costs, and managing profitability battered by shifts in payor mix driven by the pandemic, has cast focus on the efficiency and effectiveness of the current workforce structure,” said Cathy Loose, Managing Principal, SullivanCotter.
Thoughtfully defined career stages and job levels are the foundations for building a workforce architecture. SullivanCotter’s 2021 survey data indicates that almost one-quarter of titled managers do not have any staff accountability, which suggests that clarifying job definitions is a critical step many organizations miss. Then, carefully considering the desired workforce distribution within each functional area is a key pivot point that can inform the level of managerial span of control needed, define the overall size of the workforce, and influence the affordability and effectiveness of different pay philosophies.
Boardroom Focus on Demographics is Accelerating
There are few topics getting more attention from health care organization boards today than diversity and inclusion. Objectively, there are documented and researched benefits to expanding the representational diversity in the workforce. “In today’s constricted labor market, many organizations are focused on diversity as defined by race and gender, yet they are also revisiting legacy job requirements that may be limiting the diversity of experience, thought and skill in the candidate pool,” said Nanci Hibschman, Managing Principal, SullivanCotter.
SullivanCotter’s data reveals that almost one-quarter of the active healthcare workforce will reach retirement age eligibility in the next ten years. While this will create a significant challenge in terms of accelerating the pace of staff replacement, the industry has a strong foundation of diversity to build upon with over three-quarters of the workforce being female and almost one-third ethnic minorities as indicated by SullivanCotter’s data.
Healthcare organizations have a unique opportunity to lead change and influence the profile of the workforce of the future. Giving fair consideration to candidates with diverse backgrounds, experiences, knowledge, skills and abilities gives the organization the opportunity to discover new workforce combinations that may change how jobs are defined, how teams work together and how value gets created.
Considerations for 2022 and Beyond
As hospitals and health systems plan for what lies ahead and look to support financial sustainability and mitigate risk, organizations should consider market practices as well as their individual financial circumstances and structural definitions when determining their compensation and workforce-related actions.
To support more sophisticated benchmarking and customized workforce design, SullivanCotter has developed a robust statistical analysis which integrates our extensive workforce demographic and structure data with our financial, performance and quality data. This enhanced methodology produces client-specific predictive modeling of workforce size, distribution and cost customized by job family to support large-scale workforce planning and analysis.
“SullivanCotter’s 2021 Workforce Metrics Benchmark Survey reflects data collected using a rolling database model through 2020 and 2021. Due to the continued impact of the pandemic and the extremely dynamic environment, the survey data should be used thoughtfully, with appropriate context, and with sound business judgement as you plan and consider workforce management initiatives in 2022 and beyond,” said Roth.
For more information on SullivanCotter’s 2021 Health Care Workforce Metrics Benchmark Survey or any other SullivanCotter surveys, please visit our website at www.sullivancotter.com, email us or contact us by phone at 888.739.7039.
About SullivanCotter
SullivanCotter partners with healthcare and other not-for-profit organizations to understand what drives performance and improve outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, data and technology products to help organizations align business strategy and performance objectives – enabling our clients to deliver on their mission, vision and values.
READ ON NEWSDIRECT
INFOGRAPHIC | Advanced Practice Provider Leadership Compensation Practices
As the advanced practice provider (APP) workforce continues to evolve, many health systems and medical groups are developing intentional, consistent operating models for APP utilization. Consequently, APP leader roles have emerged to help oversee day-to-day clinical operations, support workforce planning initiatives and drive overall APP strategy at the executive level.
Putting APP leaders in place can help organizations improve efficiency by centralizing and standardizing key processes such as credentialing, privileging, and onboarding. APP leaders can also help reduce turnover, enhance APP engagement and satisfaction through better workforce representation on organizational committees, and improve profitability. Recent data show that organizations with APP leaders see 2% less APP turnover than organizations without this role. With the cost of turnover estimated to be between $85,832 - $114,9191, this could have a significant financial impact.
DOWNLOAD INFOGRAPHIC