Using CMS Star Ratings to Drive Improvement at Specialty Hospitals
Using national benchmarks to drive quality performance
DOWNLOAD FULL ARTICLE
In order to remain competitive in an increasingly complex marketplace, health care organizations must develop a greater understanding of what drives performance and improves outcomes in the transition from volume to value. Although the overall aim to enhance patient satisfaction, improve quality and reduce the cost of care is the same, specialty hospitals, academic medical centers, community hospitals, and major and minor teaching hospitals each operate under very distinct circumstances.
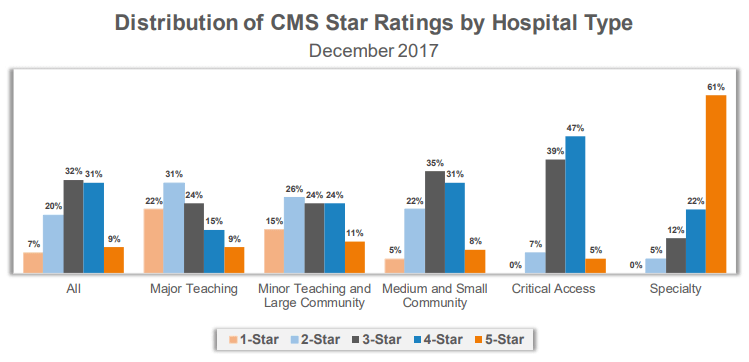
The conditions they treat are as different as the populations they serve and it cannot be assumed that patient experience at one type of hospital will be commensurate with the other. The Centers for Medicare and Medicaid Services (CMS) published its most recent Star Ratings in December 2017. While designed to measure and report hospital quality, these ratings have provoked a number of questions and concerns as more than 3,600 hospitals – regardless of size, breadth of services, or geographic location – are benchmarked against a collective average. The complexities and nuances of the new ratings can make it difficult for hospitals to truly understand how they compare to their peers and where there are still opportunities for improvement.
CMS defines specialty hospitals as those that are primarily or exclusively engaged in the care and treatment of patients with a cardiac condition; patients with an orthopedic condition; or patients receiving a surgical procedure. While CMS bases these ratings on 57 different quality measures across seven areas of performance, specialty hospitals only reported an average of 27.2 of the 57 measures. For example, 97% of specialty hospitals reported patient experience metrics. On the other hand, only 5% of specialty hospitals reported data on acute ischemic stroke 30-day mortality and 30-day readmissions because they do not typically treat this condition.
The same is true for patients with complex medical conditions such as pneumonia, coronary artery bypass graft, chronic obstructive pulmonary disease and acute myocardial infarction. Only 20-25% of specialty hospitals that were rated included measures for mortality and/or readmissions for this patient population. Additionally, less than 25% of specialty hospitals reported data for the majority of the NHSN infection rates in the Safety of Care measure group, excluding C. Difficile. The CMS ratings require additional stratification by hospital type in order to paint a more accurate picture regarding how organizations are performing in relation to their direct peers.
However, the impact of further stratification could be significant for specialty hospitals as 83% of the 74 specialty hospitals included received a four- or five-star rating. With a small number of metrics to report, specialty hospitals have fewer variables to address to help improve their scores within this ranking system and, more importantly, the care delivered to patients that can be benchmarked with publicly-reported data. All hospitals, including specialty hospitals, need to understand their variation to national benchmarks as well as the variation to their peers.
Specialty hospitals using CMS Star Ratings to drive improvement efforts should focus on the following steps:
DEFINE YOUR PEER GROUP
In addition to reviewing benchmarks for like hospitals, specialty hospitals must also consider how their ratings compare to other relevant local and regional competitors. Patient experience scores, for example, can vary widely by region. As the highest weighted measure in the CMS Patient Experience group, “Overall Rating of Hospital” had a national average of 89.01 in the December 2017 Star Ratings. On average, Nevada hospitals show a linear score of 86.90 while Wisconsin hospitals show a linear score of 90.78 – a 4.5% difference between the two states. Regional differences are important to consider when evaluating performance compared to a set of benchmarks.
BENCHMARK YOUR PERFORMANCE AGAINST PEERS
Do not underestimate the importance of peer group selection. Not all hospitals are the same – and to truly identify areas of meaningful improvement, hospitals must be compared to like hospitals. Hospitals will often have more than one peer group. For example, a specialty orthopedic hospital will want to benchmark itself against other orthopedic hospitals. However, it might also want to benchmark specific metrics like patient experience against other local hospitals that offer orthopedic services.
IDENTIFY AREAS FOR IMPROVEMENT
It is critical that organizations develop a better understanding of their variation to the CMS benchmarks. If a specialty hospital is performing above or below average, the key is to identify ‘how’ and ‘why’. Individual metrics that have a negative variance to peer group benchmarks highlight potential opportunities for improvement. Additionally, identifying areas that are important to patient outcomes and the mission of your organization will resonate most with staff and have a higher likelihood for improvement.
ALIGN REWARDS WITH TARGETED IMPROVEMENTS
Once an organization selects a specific area to target in improvement efforts, it is important to determine how employees can be motivated or incentivized to engage in these activities. As organizations shift from volume to value, quality metrics are becoming more prevalent in provider compensation plans. For example, according to SullivanCotter’s Physician Compensation and Productivity Survey, quality incentive compensation for physicians increased in 2017 from an average of 5.9% to 7.4% of total cash compensation. Aligning quality improvement efforts with compensation is an effective approach to driving change and helping to reach overall organizational goals.
REEVALUATE REGULARLY
While it is difficult to generate significant progress on one metric in a single year, organizations should not overlook the need to review these benchmarks in aggregate on a periodic basis. If there is a noticeable shift in the data, changing direction and adjusting improvement efforts accordingly is important.
CMS Star Ratings continue to provide transparency in health care quality and performance as the industry maintains its focus on value-based care. Perhaps the adage that best applies is “you can’t improve what you can’t measure” – and these ratings are certainly a step in the right direction. Despite the myriad of differences in the 3,600+ hospitals included in the CMS ratings, all share a common goal of advancing the overall quality of health care. However, to truly drive improvement and help organizations more effectively benchmark performance, the market requires a standard set of national quality metrics that is stratified by hospital type.
Organizations like the National Quality Forum and others are helping to establish these national benchmarks. Standardizing the process would help to facilitate more meaningful comparisons, allowing specialty hospitals to focus more on individual opportunities for improvement and less on their variance from the collective national average.