Optimize reimbursement by aligning physician compensation more closely with value-based payer incentives.
Since the passage of the Affordable Care Act in 2010, the Centers for Medicare and Medicaid Services (CMS) has sought to transform the U.S. health care system from one that incentivizes volume to one that rewards value. This includes a shift from fee-for-service payments to mechanisms that link provider reimbursement to improved quality and reduced costs.
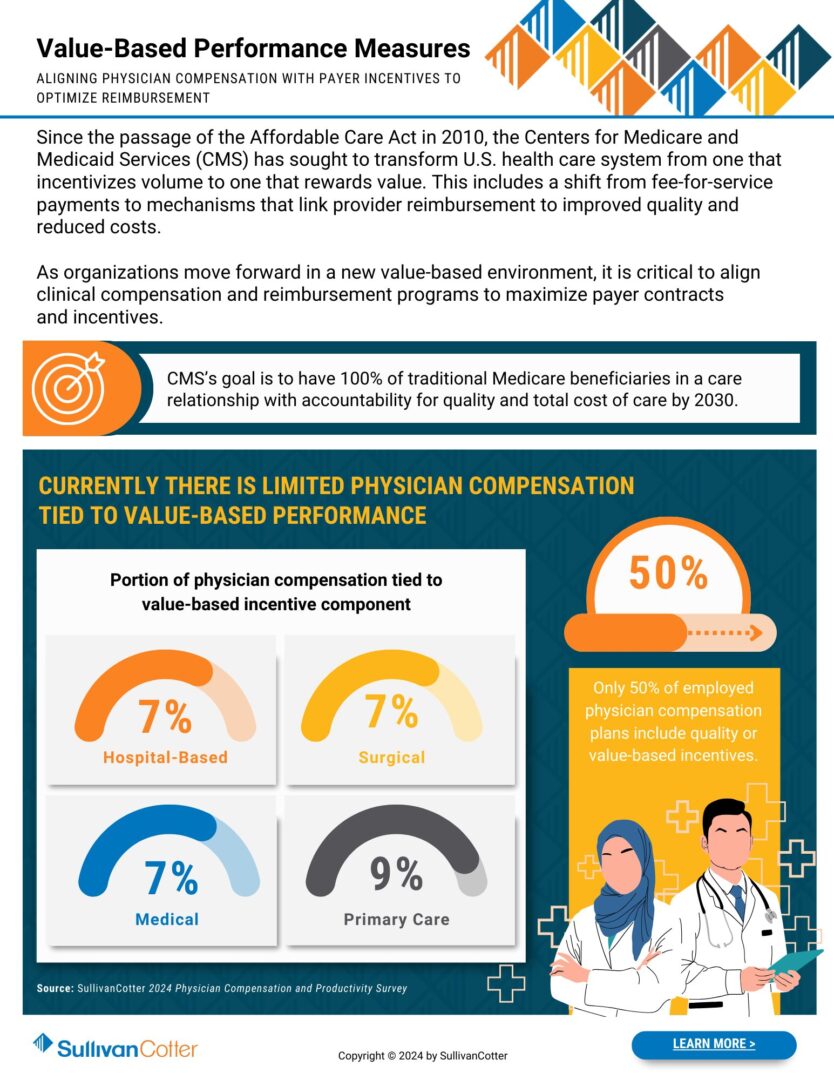
As organizations move forward in a new value-based environment, it is critical to align clinical compensation and reimbursement programs to maximize payer contracts and incentives.
CMS’s goal is to have 100% of traditional Medicare beneficiaries in a care relationship with accountability for quality and total cost of care by 2030.
Where does your organization stand?
Download our infographic to learn more about incorporating value-based performance measures into your design process.