CASE STUDY | The Value of APPs in Driving Organizational Performance
Advanced practice providers (APPs) are one of the fastest growing workforces in health care.
DOWNLOAD CASE STUDY
THE SITUATION
Advanced practice providers (APP) are one of the fastest growing workforces in health care. Not only has the APP workforce more than doubled in the last 15 years, but physician assistants and nurse practitioners are also ranked as the third and fourth best overall jobs in 2018 by U.S. News & World Report.
The focus on team-based care continues to intensify. In order to truly help transform care delivery, the role of APPs must be more clearly defined to better partner with physicians. Health systems and medical groups nationwide seek to drive better performance as the industry transitions from volume- to value-based care, and achieving the strategic goals of access, quality, affordability and provider satisfaction is a top priority.
As one of the top 10 largest children’s hospitals in the country and Arizona’s only pediatric quaternary care hospital for high acuity, complex conditions, leadership at Phoenix Children’s Hospital (PCH) recognized the need to utilize APPs more effectively to help transform patient care delivery.
Like many organizations, the number of APPs had grown swiftly and organically without a comprehensive strategy to support its sustainability. PCH realized that while they employed almost 100 APPs representing nearly $10 million in payroll, the lack of strategy had created obstacles regarding recruitment, utilization and job satisfaction. This left the organization unable to tap into the full potential of their rapidly growing APP workforce.
PCH partnered with SullivanCotter to develop a comprehensive workforce strategy to integrate, optimize and engage APPs in achieving the organization’s goals of increasing access, quality, affordability and provider satisfaction.
THE APPROACH
Senior leadership at PCH collaborated with a team of advisors from SullivanCotter to assess the utilization of their current APP workforce and developed a systemic approach to redesign care models and build the culture and infrastructure necessary to support the optimization of APPs.
Supported by decades of clinical and operational health care industry experience, as well as proprietary APP data on utilization, compensation and leadership structures, SullivanCotter provided unique insight into the evolving role of the APP and the challenges health systems and medical groups face when trying to utilize this workforce more effectively.
“Medical group, hospital and nursing executives must be fully aligned and work together
throughout the entire process to ensure the optimization and engagement of all team
members, including physicians, advanced practice providers, registered nurses and
medical assistants.”Dr. Jared Muenzer, MD, MBA
Senior Vice President and Chief Operating Officer, Phoenix Children’s Medical Group
The approach included three phases: education and assessment, program design, and implementation.
A number of PCH leaders were involved throughout the process – including the CEO, CMO, COO of the medical group, SVP/CNO, Surgeon in Chief, executive general counsel, and physician and APP leaders. Physicians were also meaningfully engaged in the assessment and design and led the implementation efforts in their divisions.
To start, all APPs were surveyed to learn more about their current utilization and perception of the culture at PCH. Key policies were also reviewed to assess current practices compared to federal and state regulations as well as national trends and leading practices.
Findings from the initial assessment uncovered the following:
- Only 42% of APPs felt they were being utilized to their maximum potential
- APPs were performing many activities that could be completed by other team members such as RNs, MAs or social workers
- Medical staff bylaws were more restrictive than state law or CMS requirements
- Clinical privilege lists were out of date
- There was no formal orientation program for APPs, though over 40% were hired as new graduates
- APPs received limited education on documentation and billing
- Multiple key stakeholders desired clarification on the NP and PA scope of practice
Using the findings from the assessment, SullivanCotter worked with PCH executives and physicians to develop a list of guiding principles. To help inform a comprehensive APP strategy, the organization determined it must:
- Define models of care based on patient needs and clinical specialty
- Ensure providers work to their full potential and support top-of-license practice
- Bill based on service provider
- Build a culture and infrastructure to support the utilization, retention and engagement of APPs
- Measure progress to ensure sustainability and identify new opportunities for improvement
- Develop a provider workforce plan that includes APPs in addition to physicians
Facilitated by SullivanCotter, these guiding principles were then used by multiple clinical divisions (cardiac surgery, CVICU, cardiology, emergency services, urgent care, orthopedics, urology, gastroenterology and transplant) to re-examine and redefine the role of APPs in patient care delivery.
Additionally, other project teams were enlisted to help ensure the continued optimization and engagement of the APP workforce. They focused on the development of new:
- Leadership structures
- Privileging and competency assessment (FPPE/OPPE) processes
- Onboarding processes with clearly defined roles for preceptors and physicians
- Documentation and billing education and guidelines
- Marketing and branding approaches more inclusive of APPs
The progress of the clinical and operational implementation was monitored by an executive steering committee on a quarterly basis through scorecards for each committee and clinical specialty.
“This process has produced clear and compelling results to reinforce the idea that APPs can
help drive organizational performance and improve outcomes. This is critical in an emerging
value-based health care environment and is necessary to meet the growing demand for
highly-trained health care providers.”Julie Bowman, MSN, RN
Senior Vice President, Patient Care Services and Chief Nursing Officer, Phoenix Children’s Hospital
THE RESULTS
The PCH leadership team understood that APPs were a valuable but underutilized resource and championed the optimization of this workforce as a key organizational strategy. This helped to improve access and health outcomes for its patients and achieve its goals for expansion and financial performance. Over a two-year period of redefining their care models and implementing the strategy, PCH was able to accomplish the following:
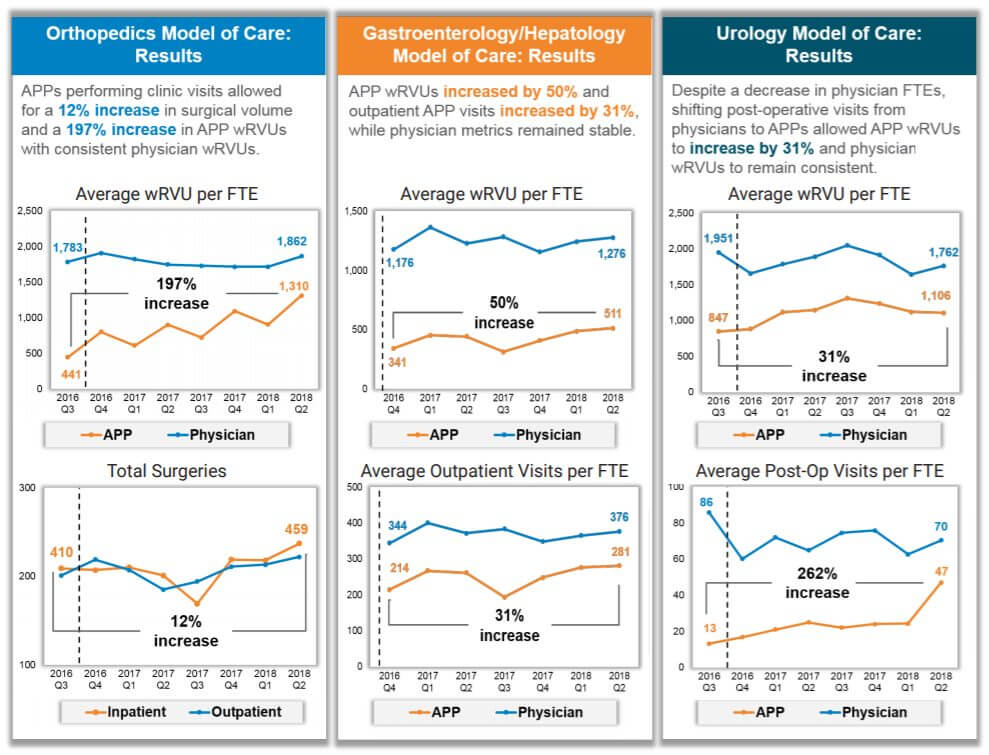
- In orthopedics, a 197% increase in APP wRVUs with no decrease in physician wRVUs, and a 12% increase in surgeries (productivity and revenue) with no additional staff
- In gastroenterology, a 50% increase in APP wRVUs with slight increase in physician wRVUs, a 31% increase in APP outpatient visits and a 9% increase in physician outpatient visits (productivity and access)
- In urology, a 31% increase in APP wRVUs with slight decrease in physician wRVUs due to a decrease in physician FTEs, and over 250% increase in APP post-operative visits
- In less than a year, reduced time to fill APP positions by 50% (down from 79 days to 38.5 days)
- APP turnover decreased by an average of 47% since 2016
- Implemented a comprehensive onboarding program for APPs that was also adopted for new physicians
- Added APP representation to multiple medical staff committees
LESSONS LEARNED
As health systems and medical groups consider developing their own APP strategies to improve the way care is delivered in today’s evolving market, PCH’s model is transferrable to both pediatric and nonpediatric organizations. There are a number of key lessons learned from PCH’s journey for other organizations to consider.
The following guidelines are essential to the implementation process:
- Ensure active participation and engagement from hospital, medical group, nursing and executive leadership throughout the process
- Identify physician champions early on
- Care model redesign must focus on all team member roles, including physicians, APPs, registered nurses, medical assistants, care managers and more
- Align physician and APP performance management, compensation and incentive plans
- Ensure some early successes
- Conduct regular key stakeholder meetings to provide updates on progress
- Agree upon implementation plan and hold key physician, APP and service line leaders accountable
About Phoenix Children’s Hospital
Phoenix Children’s Hospital (PCH) is one of the 10 largest children’s hospitals in the country and Arizona’s only “Best Children’s Hospital,” ranked in all 10 specialties by US News & World Report. This includes a 433-bed acute care facility with 18 clinical divisions and six sites of care serving pediatric inpatient, outpatient, urgent care, emergency and trauma services. In 2015, Phoenix Children’s Hospital had 18,773 inpatient admissions, 80,514 visits to the Emergency Department, 237,514 outpatient visits, and 16,491 surgical cases.
In 2017, Phoenix Children’s Hospital received the Phoenix Business Journal’s prestigious HealthCare Leadership Award and was named to Best Companies AZ’s “100 Best Arizona Companies” list for health care. An internal survey placed the hospital in the 90th percentile for employee satisfaction.