Physicians: 2021 Evaluation and Management CPT Codes
Part I: Understanding the Impact on Physician Compensation
DOWNLOAD FULL ARTICLE
Updated: February 2021
RELATED CONTENT:
PART II: 2021 E&M CPT Code Changes: Addressing the Impact on Advanced Practice Providers
INFOGRAPHIC | Considerations for Addressing the 2021 E&M Work RVU Changes
ARTICLE | Navigating Change: Implications of the 2021 Physician Fee Schedule
Every year, the Centers for Medicare and Medicaid Services (CMS) evaluates the recommendations of the American Medical Association’s (AMA) Relative Value System Update Committee (RUC) and conducts its own review of the Work Relative Value Unit (wRVU) values associated with each Current Procedural Terminology (CPT) code to determine if wRVU revisions are needed based on the time, skill, training and intensity necessary to perform each service.
The degree of change varies from year to year, and the impact on individual specialties depends on which codes are modified and the extent to which the values are adjusted. CMS has issued the 2021 Physician Fee Schedule final rule and has significantly overhauled the Evaluation and Management (E&M) code documentation requirements, time-effort recognition, and wRVU values for face-to-face new and established patient office visits. These changes were effective as of January 1, 2021.
Many physicians provide office-based E&M services and, when broad changes such as this occur, the resulting impact can be significant. This article will address:
- CMS efforts to recognize increased work effort for office visits as well as a summary of the 2021 changes to E&M codes.
- The reimbursement impact on Medicare physician services as well as the likely downstream effect on commercial payer physician reimbursement.
- The potential impact on physician and advanced practice provider (APP) reported productivity levels for various specialties.
- The potential unintended impact on compensation arrangements – especially wRVU production-based plans or salary-based plans with wRVU-based performance measures.
- Other variables that could influence the assessment of your organization’s wRVU productivity.
PHYSICIAN AND APP WORK RESPONSIBILITIES FOR E&M OFFICE PATIENT VISITS
“Patients Over Paperwork” is a CMS initiative based on the AMA’s RUC recommendations. The goal of this initiative is to reduce burdensome regulations, enhance efficiency and improve the physician experience. The E&M review and adjustments are steps towards removing regulatory obstacles that impede a clinician’s ability to spend time with patients. The first wave of this initiative includes the modification of ten E&M codes used for billing new and established office-based patient visits (codes 99201-99215). Other E&M code groupings (inpatient, skilled nursing, etc.) will be reviewed at a future date.
Several factors were considered when formulating the 2021 changes including:
- To maintain the “Patients Over Paperwork” goal, CMS kept the documentation reduction requirement for appropriate coding.
- CMS estimates that these adjustments will save 180 hours of paperwork for physicians annually.
- A time study commissioned by CMS determined that, due to the added responsibilities physicians have experienced over the last five years, an increase in wRVUs for many E&M codes is justified. These include:
- Longer patient face-to-face time during visits.
- Increased non-patient time responsibilities such as Electronic Medical Record (EMR) documentation.
- Added non-reimbursed physician time to coordinate team-based care and population management.
- To recognize the occasional extended time patient visit, CMS incorporated an add-on code (G2212) for every 15 minutes of additional work effort beyond the time expectation associated with codes 99205 and 99215.
- This extended time method is similar to anesthesiology work value measurement that credits added time units along with the base procedure.
- Implementation of another add-on code (G2211) has been deferred until January 1, 2024. At that time, an add-on code will be available to provide additional recognition (reimbursement and wRVU credit) for qualified, severe, or complex chronic patient conditions.
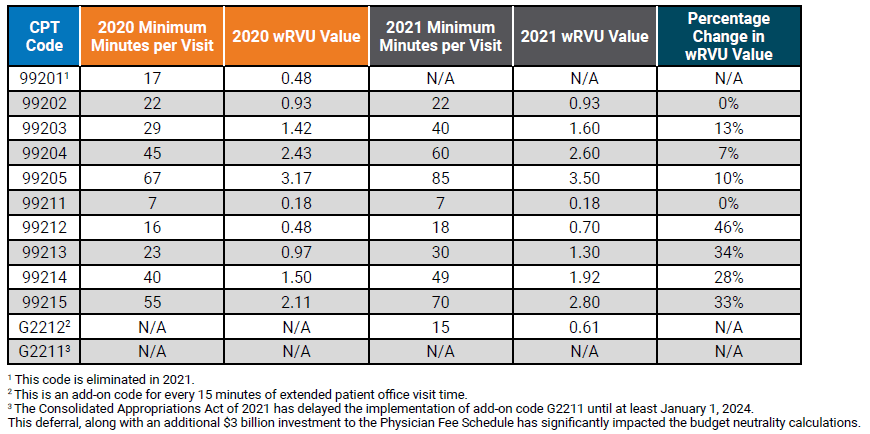
These adjustments, along with CMS quality incentive payments, signify CMS’ increased recognition of how the process of delivering high-quality health care has changed. The impact of these changes will result in material increases in reported wRVU productivity for office-based specialties. Table 1 below compares the 2020 and 2021 E&M code time allocation and wRVUs.
Table 1: Time Allocations and wRVUs Adjustments: Current versus 2021
THREE IMPORTANT POTENTIAL IMPACTS TO PHYSICIAN PRODUCTIVITY LEVELS AND RESULTING COMPENSATION AND BENCHMARK MEASUREMENTS
1. How will the 2021 wRVU changes impact the measurement of physician productivity?
This is often the first question that arises when organizations try to assess how wRVU changes will impact reported productivity internally, but also when comparing to published national survey benchmarks. To help analyze the impact, SullivanCotter utilized its proprietary database consisting of individual CPT code volumes and modifiers for approximately 20,000 physicians across 100 different specialties. We recalculated two versions of wRVU productivity for comparison: one based on the 2020 wRVU values, and one based on the new 2021 wRVU values. By keeping volumes and distribution constant, the change in reported wRVU productivity is entirely due to the 2021 wRVU adjustments.
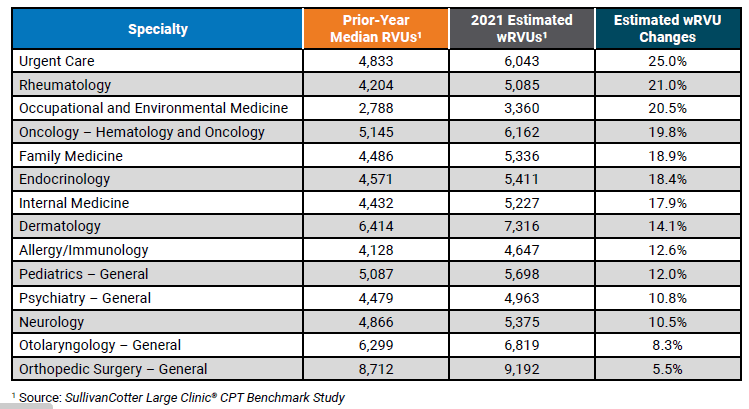
Summary findings indicate that of the 100 specialties reviewed, wRVU benchmarks for 46 specialties increased between 3% and 11%. The modeling shows that wRVU benchmarks for an additional 25 specialties increased by greater than 11%. Table 2 below shows the resulting impact on reported wRVUs by number of specialties. This represents a significant change to wRVU benchmarks, and it will be important for organizations to understand the impact on physician compensation and physician practice economics.
Table 2: Overall Specialty Impact of 2021 E&M Code Changes
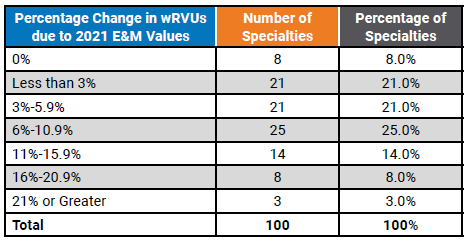
Table 3 below illustrates a sample of some of the individual specialties with notable increases to reported wRVUs.
Table 3: Median wRVU Impact of 2021 E&M wRVU Changes
2. How will wRVU changes impact physician compensation benchmarks?
The answer to this question depends on the structure of an organization’s compensation program. If a plan is based heavily on historical compensation per wRVU benchmarks, there will be, all this being equal, an immediate increase in the amount of compensation paid to physicians as a result of the change in wRVU values. According to SullivanCotter’s 2020 Physician Compensation and Productivity Survey, nearly 3/4 of organizations indicated that wRVU productivity drives more than 50% of physician total cash compensation. Conversely, physicians with salary-based plans linked to national compensation benchmarks will not experience an immediate increase in compensation but may experience a change over time as benchmarks evolve.
Over 95% of the organizations participating in the survey utilize national benchmarks to determine annual salaries and/or compensation per wRVU rates. Understanding how to use these benchmarks appropriately is/will be important during the 2021 and 2022 transition years.
SullivanCotter reviewed several different compensation methodologies to estimate the potential impact to survey benchmarks. Considering the E&M code wRVU changes and assuming no modifications are made to compensation plan methodologies we estimate average clinical compensation will increase by approximately 6% assuming no changes in compensation rates is made. This analysis does not include implications from other market factors such as demand, inflation, cost-of-living, changes in productivity and more. As with reported wRVUs, this impact will vary significantly by specialty. Table 4 below highlights the estimated changes to survey benchmarks. See Column A to find the estimated change in compensation.
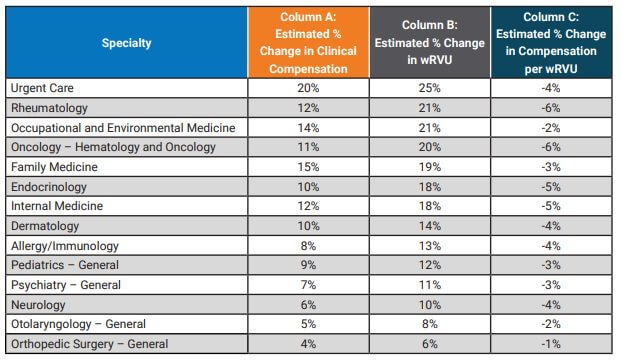
If an organization utilizes wRVU productivity targets to determine compensation using the 2020 survey data while calculating wRVUs using the 2021 wRVU schedule, this will result in higher compensation as physicians meet or exceed the production targets at an increased rate.
Similarly, if an organization uses the 2020 compensation per wRVU survey benchmark while using the CMS 2021 values to calculate physician productivity, clinical compensation will increase as a result of using compensation per wRVU rates calculated on the older (lower) wRVU values. Using Internal Medicine as an example, the following graph represents the potential unintended consequences for organizations using a variety of compensation plan designs assuming no change in compensation plan methodology. The potential impact varies significantly depending on whether an organization primarily utilizes a wRVU incentive plan versus a salary-based plan.
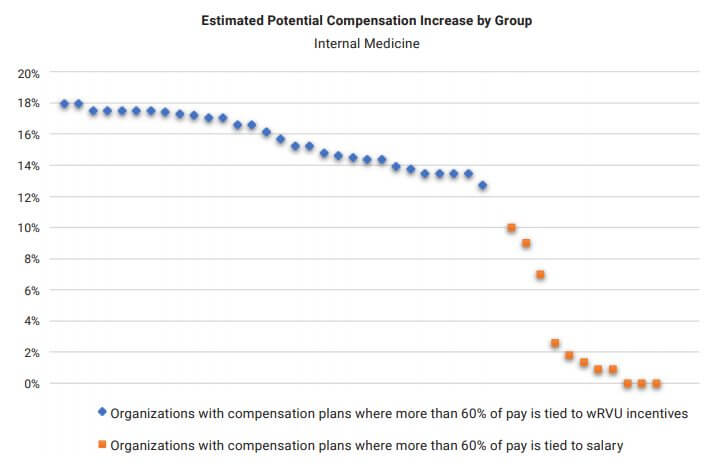
To avoid these pitfalls, organizations should conduct a strategic review of the 2021 Physician Fee Schedule changes to determine the impact on their physician compensation plans. Considerations include awareness, appropriateness, affordability and feasibility of modifications as well as physician expectations regarding any potential change in compensation.
3. If organizations utilize compensation per wRVU benchmarks, what should they expect with regard to the 2021 survey benchmarks?
As mentioned above, nearly 75% of organizations in the SullivanCotter 2020 Physician Compensation and Productivity Survey utilize the compensation per wRVU benchmark in determining physician compensation. For any organization using the 2021 wRVU values in their compensation plan, a fundamental understanding of how market benchmarks will change is important.
In this article, we reviewed estimated increases to both wRVUs and clinical compensation. However, because the expected change in wRVU values exceeds the expected change in clinical compensation, compensation per wRVU ratios are expected to decrease in future surveys. See Column C in Table 4 for the estimated impact on specific specialties. Overall, our study indicated a 3% decrease in the TCC per wRVU rate, but with significant variability by specialty.
OTHER FACTORS TO CONSIDER WHEN ANALYZING COMPENSATION IMPACTS
As organizations continue to evaluate the impact of the final rule during this industry transition, there are several other factors to consider. These include:
- Will moving forward with historical compensation per wRVU rates and 2021 wRVU values unintentionally create Fair Market Value (FMV) and Commercial Reasonableness (CR) risks due to the resulting higher compensation payments?
- Do compensation incentive plans include supervisory payments to physicians based on APP productivity levels? The 2021 wRVU value changes will also affect codes utilized by APPs.
- For specialties that are paid shift rates, are there additional incentive opportunities based on wRVU productivity?
- Does the organization pay for physician virtual care visits by tying them to office visit E&M values? This could result in unintended higher pay for virtual care.
- CMS has added G2212 as an add-on code intended to be used with 99205 and 99215 for each additional 15 minutes above 70 minutes of documented time associated with an individual patient visit. The assumptions and analysis above do not account for changes in the distribution of E&M coding or increases in reported wRVU productivity due to this new code. A wRVU increase does not automatically equate to an equal reimbursement increase.
- CMS also applied an annual budget neutrality factor which caps overall physician fee schedule reimbursement to avoid a significant increase in CMS payments. The reduction in the CMS conversion factor, in combination with significant increases in wRVUs for cognitive specialties, may result in additional compensation paid to physicians. However, revenue increases are unlikely to offset the more significant increases in wRVU-based compensation if 2021 E&M code values and historical compensation per wRVU rates are utilized going forward.
The published 2021 Physician Fee Schedule final rule reduced the Medicare conversion factor by 10.2% to maintain statutorily required budget neutrality. However, on December 27, 2020, the Consolidated Appropriations Act of 2021 – including provisions that temporarily mitigate a portion of the conversion factor reduction – was signed into law. The CMS final rule tables were later published with the 2021 Medicare conversion factor set at $34.89. This is a reduction of 3.3% from 2020. However, expected Medicare revenue increases resulting from the combination of higher RVU values and a higher than anticipated conversion factor rate, are unlikely to offset the more significant increases in wRVU-based physician compensation absent any change in compensation plan rates going forward.
SullivanCotter offers advisory support and technology solutions to help your organization understand and respond to the potential impact of these changes.
To learn more, contact us at 888.739.7039 or info@sullivancotter.com