CASE STUDY | Strategies for Addressing Radiologist Supply Shortages
Recommendations to help your organization to maintain adequate coverage
by Dave Hesselink, Managing Principal, SullivanCotter and Tim Stamper, Principal, SullivanCotter
The field of diagnostic radiology is undergoing significant transformation driven by advancements in technology, the increased demand for imaging to support cancer patients, and the integration of artificial intelligence (AI) into key workflows. As imaging becomes increasingly central to patient care, health systems are working to ensure their staffing models for this key service line are highly functioning as related challenges and opportunities arise.
Presented via a series of case studies, this article illustrates key obstacles many organizations are facing as the demand for radiologists continues to grow but the supply of providers falls short. Given the implications these shortages could have on patients and the broader medical community, this issue has raised concerns among health care providers across the nation. As health systems look to address these challenges and maintain coverage, many are reevaluating the way they contract, employ, and compensate radiologists.
Market Perspective and Changing Landscape
According to the American College of Radiology (ACR), the demand for diagnostic imaging services is rapidly increasing. This is driven by an aging population, chronic disease management, and the growing reliance on imaging for diagnosis and treatment planning. However, the supply of radiologists is not keeping up with this demand. The ACR reports that the shortfall could reach as high as 19,500 radiologists by 2036.
This shortage is further compounded by an aging radiologist workforce and limitations on new entrants into the field.2 In other fields of medicine, other clinicians such as advanced practice providers have been critical in helping to improve or maintain patient access amidst ongoing physician shortages. However, in diagnostic radiology, there is no equivalent alternative workforce available. Organizations are also facing several recruitment and retention challenges within this specialty as professionals can be more selective in a competitive job market that includes non-traditional options like teleradiology. Additionally, there is growing concern that technological advancements, such as AI and automation, cannot fully replace the expertise and decision-making capabilities of human radiologists. As the shortage continues to grow, the ACR is calling for action to address this gap through measures such as expanding training programs, promoting workforce representation, and leveraging technology to enhance the efficiency of radiological services.
The ACR also notes the challenges faced by regional private radiology groups in its research.3 The decline of these groups has been attributed to several factors – including consolidation within the health care industry, financial pressure from declining reimbursement, the rise of corporate-owned radiology groups, and the growing complexity of managing practices in a competitive job market. These pressures are leading to concerns about the shrinking number of independent radiology practices and the impact this may have on job satisfaction, autonomy, and the quality of patient care.
How are Organizations Addressing These Issues?
Please note these are real organizations with fictional names.
Case Study #1: Radiology Coverage for a Midwest Community Hospital
Midwest Community Hospital (Midwest) is a 400-bed medical center that partnered with a local independent medical group (the Group) to provide diagnostic and interventional radiology services. The partnership operated under a professional services agreement (PSA) in which the Group billed for imaging services and Midwest subsidized the Group by covering the gap between the professional collections – minus Group operating expenses – and the market rate for imaging services.
In early 2024, the Group notified Midwest that it would terminate the PSA due to chronic staffing shortages and financial difficulties arising from the structure of the original agreement. As a result, Midwest was left with limited options for securing imaging services moving forward.
These options included:
- Directly employ its own radiologists
- Renegotiate the terms of the existing PSA to maintain the current Group’s coverage
- Enter into a new PSA with a national radiology firm
Midwest believed that employing its own radiologists directly was the least feasible option considering ongoing recruitment challenges and supply and demand imbalances. Although the organization attempted to renegotiate with the Group, discussions regarding the financial terms of the original PSA proved unproductive as the Group felt the arrangement was no longer sustainable due to the high market rates being requested by new recruits coupled with retention challenges among its existing workforce.
As a result, Midwest entered into negotiations with the national imaging firm and put a new PSA in place that replicated the compensation structure of their previous arrangement. However, Midwest was unaware that the national firm did not have adequate staffing and had attempted to recruit radiologists from the Group to ensure it could provide enough coverage to meet demand. This led to resistance from the Group’s radiologists – leading them to reject the firm’s recruitment efforts. As a result, the national imaging firm was forced to terminate the PSA with Midwest before it even began.
With no new options available and still without the imaging services it required, Midwest returned to discussions with the Group for providing coverage. The Group requested a completely new compensation structure that shifted from an FTE-based compensation arrangement to a work relative value unit (wRVU) compensation model. Under this new model, Midwest would assume responsibility for billing and collecting for imaging services provided by the Group and pay them a market rate per wRVU.
While this new compensation model resulted in higher costs, the hospital concluded that this was the best choice in order to serve their patient population. This decision was based on the critical need to provide uninterrupted imaging services in the future.
Case Study #2: Radiology Coverage for a Regional Hospital in the Northeast
Similar to Midwest’s experience, Northeast Regional Health System (Northeast) faced its own radiology coverage challenges under similarly difficult circumstances, but with different potential solutions.
Northeast includes a 450-bed medical center and several outpatient facilities. Regional Radiology Associates (RRA) is a 20-person radiology group that partnered with Northeast for over 50 years to provide nearly all radiology interpretations at Northeast’s hospital and three separate outpatient facilities on a 24 hours a day, 365 days a year basis. In the fall of 2024, RRA abruptly provided Northeast with 60 days of notice that it would only provide these services Monday through Friday between the hours of 8:00 AM and 4:00 PM – representing a significant reduction in service.
Given Northeast’s reliance on this arrangement, the organization swiftly engaged in negotiations with RRA to provide the required radiology coverage services on a long-term basis. Those attempts failed, however, and there were no other local radiology groups who were credentialed and able to provide the required coverage upon completion of RRA’s 60-day notice period.
As such, the organization was forced to evaluate other options. Northeast quickly secured remote radiology coverage from a national locum tenens agency from 3:00 PM to 11:00 PM seven days per week and remote overnight coverage from a national teleradiology firm from 11:00 PM to 7:00 AM seven days per week. However, hospital and payer credentialing processes were expected to take longer than 60 days to complete, so Northeast was forced to negotiate an interim PSA with RRA to provide transitional diagnostic radiology services for an additional two-month period to bridge the anticipated gap.
This led to the development of three approaches with different timelines:
The Transitional Period Solution
- RRA received a retention bonus for the continuation of diagnostic radiology coverage services during the two-month transition period. Half of the retention bonus was paid in bi-weekly installments during this two-month period and the other half was paid at the conclusion of the two-month transition period if RRA satisfactorily provided coverage – which included interpretations from 8:00 AM to 11:00 PM, seven days per week, and unrestricted on-call radiology interpretation coverage in the event of defined special circumstances (e.g., emergency fluoroscopy).
- RRA continued to bill and collect for its professional services and retained all professional collections generated.
The Mid-Term Solution
- RRA provided day-time coverage Monday through Friday while Northeast contracted with the teleradiology firm to provide coverage evenings, nights, and on weekends.
- RRA provided unrestricted call coverage for the relatively infrequent special circumstances outlined in the transitional PSA arrangement.
The Long-Term Solution
- Greater reliance on national teleradiology firms and direct employment.
- Employment will help to satisfy daytime and unrestricted call coverage requirements. However, it will take time to recruit an adequate number of employed physicians as well as the radiology leadership needed to make this long-term solution viable.
- National remote teleradiology will provide coverage on evenings, nights, and weekends.
In the meantime, Northeast finds itself in an uneasy situation and is working towards a viable long-term solution in the event RRA is no longer sustainable as a private practice partner.
Case Study #3: Radiology Compensation Model within a Safety Net Hospital
Lastly, a Safety Net Hospital (West) located on the West Coast faced unique radiology staffing challenges due to its location and desirable living conditions. West is a 4-hospital health system whose flagship hospital is a 500-bed Level 1 trauma center – the only trauma center in the region. The organization also operates three smaller hospitals in surrounding communities.
Several years ago, West began employing its radiologists to address financial issues that threatened the sustainability of the group as an independent practice. West’s diagnostic radiology volume would indicate a full staffing level of 25 FTEs is needed. However, West operates in a region that is unique due to its popularity with teleradiologists who live in the region but perform overnight reads for East Coast clients to take advantage of the time differential. Therefore, West had experienced difficulty recruiting and retaining diagnostic radiologists who view direct employment as less attractive due to more onsite and on-call requirements, unpredictable work schedules, and less elective work.
After several years of high attrition, West found itself in with only five remaining employed diagnostic radiologists. These five were supported by both interventional and breast radiologists who were pressed into general diagnostic radiology service to keep up with the growing demand. Out of necessity, the remaining five diagnostic radiologists were forced to operate at extremely high productivity levels and were producing wRVUs at twice the 90th percentile level nationally. After a number of failed recruitments and in the face of potentially dire consequences such as the diversion of ER cases to local competitors, losing cancer accreditation, and legal challenges due to delayed diagnoses, leadership quickly negotiated a per wRVU teleradiology agreement with a national vendor for 24/7/365 interpretation coverage on an as-needed basis for up to 100% of its diagnostic radiology needs. This came at a significant cost.
West’s leadership recognized that executing on its preferred long-term strategy could not be accomplished overnight. To account for this, leadership developed a short-term strategy that utilized a new compensation plan for employed physicians that was locally competitive. It also needed to support the recruitment and retention of high performers. West’s employed compensation plan set base salaries at the 75th percentile for new recruits and included a ‘hardship’ retention bonus of $150,000 annually for physicians producing at or above the 80th percentile RVU productivity level. When added to base salary, this resulted in TCC at the 90th percentile nationally. Leadership pitched the ‘hardship’ retention bonus as a temporary measure that will be in place only until enough new diagnostic radiologists can be recruited and productivity expectations return back to a normative market level. West’s recruitment success to the new employed compensation model is still undetermined.
Due to the significant cost associated with the national teleradiology firm coverage arrangement, leadership viewed it as a temporary backstop while it developed and executed a longer-term radiology workforce strategy. The strategy called for rebuilding the employed diagnostic radiology group over time by emphasizing work-life balance and avoiding excessive productivity.
Knowing this would take several years to execute, the organization’s mid-term strategy included:
- Protecting interventional radiologists from being utilized in diagnostic radiology roles by securing the services of the national teleradiology firm.
- Establishing a local hybrid model of both onsite and remote diagnostic radiology work
- Employing teleradiologists on the East Coast to take advantage of the time zone differential
- Utilizing the national teleradiology contract during high-demand periods, as necessary for specialty needs, and to perform off-hours reads.Developing a decentralized diagnostic radiology team through:
What’s Next?
While the responses undertaken by these three health systems are instructive, they are also reactionary – which often leads to higher costs and potential compromises in care delivery. Given the current environment, it’s important that health systems take proactive steps now to avoid potential crisis situations.
Those steps include:
- Reviewing current radiology coverage arrangements to understand notice provisions and identify potential vulnerabilities inherent in relationships with independent groups.
- Maintaining communication with radiology partners to ensure that current PSAs are meeting the needs of both parties. If not, be proactive in understanding what needs to change.
- Consider alternative compensation models as opposed to defaulting to standard coverage agreement terms. Radiology groups are currently running lean by doing more with less providers and want to be rewarded for improving efficiency and productivity.
- Monitoring the ongoing radiology market to ensure compensation plans and workload expectations for employed radiologists remain market competitive. Employed coverage models are still susceptible to market forces and, even with even a modest amount of attrition, can quickly spiral into larger problems.
- Executing an overflow coverage contract with a teleradiology firm to maintain diagnostic radiology service levels if attrition of employed radiologists gets too high.
- Protecting interventional radiologists may be necessary to avoid a secondary crisis where interventional radiology coverage is threatened due to diagnostic radiology demands.
- Maintaining employment settings and expectations that are attractive to candidates in the face of teleradiology options – which offer recruits more control over their schedule, work from home, and no on-call responsibilities. Health systems should consider how their work settings can be made more attractive to potential candidates. Subspecialty focus, mentorship, and group collegiality are all strategies that can be used to maintain employment as an option for long-term success and stability.
Conclusion
The field of diagnostic radiology is at a critical juncture as organizations face a shortage of imaging professionals. This issue is simultaneously being exacerbated by an aging workforce, evolving technological demands, and increasing patient care needs. To address these staffing challenges, health care organizations are utilizing a number of diverse strategies – including renegotiating partnerships with independent groups, securing national teleradiology firm coverage, and developing internal teleradiology coverage.
It is essential to adopt flexible and forward-thinking staffing models that incorporate both technological advancements and innovative compensation structures as health systems navigate unprecedented workforce challenges. By fostering collaboration, embracing alternative coverage solutions, and prioritizing competitive retention and recruitment strategies, health care organizations can better position themselves to meet the rising demand for diagnostic imaging services and ensure sustainable, high-quality patient care in the years to come.
VIDEO | Determine the right number and type of physicians needed in a given market
Take a data-driven approach to workforce planning! Watch our new video for the latest insights.
Struggling to balance physician supply with patient demand in the communities you serve?
An imbalance often results in hiring the wrong number and type of providers in a given market – which can lead to workforce inefficiencies, increased costs, and issues meeting patient care needs.
Leverage market-specific data to find the right strategy!
SullivanCotter’s Mark Ryberg discusses how organizations can review and refine their physician workforce strategy by analyzing local demand, comparing it to existing provider supply, and identifying potential staffing gaps.
Access the data you need!
Explore our Provider Needs Assessment solution to analyze your local market’s physician supply and demand, identify service delivery gaps, and more!
VIDEO | How can APPs help to drive greater patient access?
Bolster your APP workforce strategy!
Learn more from our ongoing video series.
The demand for care is at an all-time high.
Is your organization doing all it can to maintain and even increase patient access? Advanced practice providers are critical in achieving these goals!
Tune into our latest video in which Hadley Powless discusses how top-of-license practice can help organizations bridge the gap between patient access and demand.
Looking for help?
We’re experts in developing strategic models of care to effectively integrate and engage this growing workforce.
Learn more about how we can help you enhance the way APPs are utilized across your organization.
PODCAST | Value-Based Care: Latest Trends and Developments
By 2030, the Centers for Medicare and Medicaid Services' goal is to have 100% of traditional Medicare beneficiaries in a relationship with accountability for quality and total cost of care.
Is your organization set up for success?
Health care organizations nationwide continue to navigate the shift from volume to value-based care. While improving clinical operations and performance to help support important quality and population health management initiatives remains a top priority, many are still finding it difficult to navigate complex regulatory requirements, manage changes in reimbursement, and align physician compensation more closely with value-based incentives.
Tune into this AHLA-sponsored podcast for the latest guidance from our experts!
SullivanCotter’s Rob Moss sat down with Maggie Martin, Chief Legal Officer at the Oklahoma Hospital Association, to explore how organizations can:
- Address any potential implications of CMS’ goal
- Compensate physicians more effectively in the transition from volume to value
- Align performance metrics with incentives with how they’re being reimbursed by payers
Forbes | What is the key to health care succession planning?
Early Strategizing and Flexibility are Key to Health Care Succession Planning
The health care industry is experiencing a critical gap in expertise as operations grow more complex and executives retire or step away.
As exits trend up, succession planning is a pressing challenge that many leading health systems in the U.S. are struggling to address.
Whether a change among top leadership roles is planned or unexpected, its impact on the rest of the organization—and how the strategy for the next generation of leadership plays out—can have far-reaching effects on a system’s financial performance, employee retention and care delivery.
There are three important considerations that organizations should take into account as they look to minimize disruption before, during, and after key leadership transitions.
Recently featured in Forbes, SullivanCotter’s President and CEO, Ted Chien, highlights care organizations must:
- Start planning three to five years early
- Hire future leaders now
- Weigh the merits of internal verus external hires
VIDEO | How have APP productivity measures evolved?
Accelerate the impact of your APP workforce with greater insight into productivity!
Learn more from our ongoing video series.
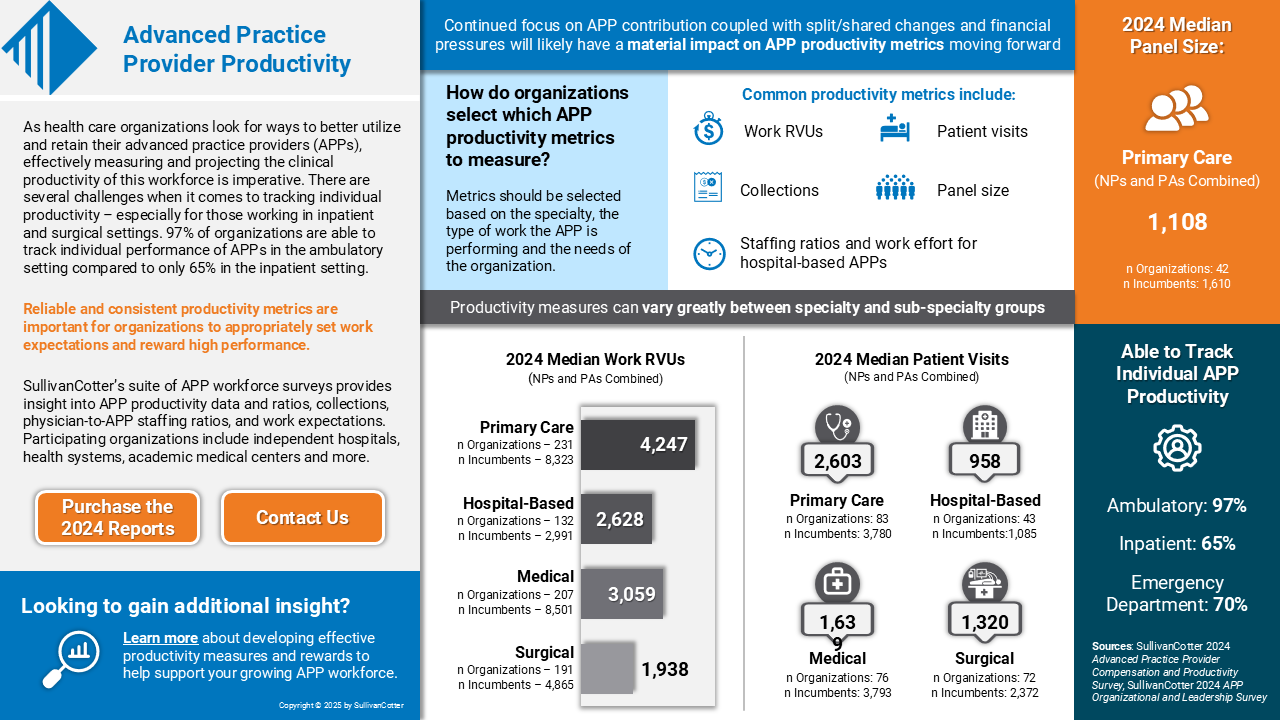
How has the measurement of advanced practice provider productivity evolved over the past few years?
Reward high performers, manage team performance, and set appropriate work expectations with reliable APP productivity data!
Both the tracking and reporting of APP productivity have evolved significantly in recent years as organizations look for better ways to monitor performance. The amount and scale of data has grown to include several different variables such as work RVUs, encounters/visits, and even quality and value-based outcomes.
Learn more from SullivanCotter’s Sarah Kasner on evaluating APP performance and how our productivity data can help you set individual and team goals.
Looking for additional insight?
We’ve got more data!
Download our infographic to access the latest APP productivity benchmarks – including wRVUs, collections, patient visits, and more.
CASE STUDY | Anesthesia Coverage: Assessing Professional Services Agreements
Is your anesthesia group struggling to meet coverage demands?
It may be time to reassess the terms of your professional services agreements (PSA) for this critical service line.
The demand for anesthesia coverage is greater than ever as staffing shortages persist and surgical procedures increase. Coupled with rising subsidies, many organizations are finding that their existing arrangements are not financially sustainable.
SullivanCotter recently partnered with a large not-for-profit health system in the Midwest to evaluate the terms and group performance under its PSA for anesthesiology at five acute care hospitals.
Discover how he worked with this client to:
- Stabilize coverage by renegotiating PSA terms to include clearer performance expectations and identifying the optimal number of anesthesiologists to satisfy current and future coverage needs, patient volumes, and staffing models.
- Improve financial performance by determining appropriate subsidy to support market-competitive and compliant compensation and identifying underperforming third-party billings/collections provider
- Enhance overall service line approach by developing a sustainable anesthesia strategy to best meet organizational goals and growth related to surgical services.
- …and more!
View the case study for greater insight into this organization’s challenges, our approach, and the outcomes!
INFOGRAPHIC | 2024 Advanced Practice Provider Productivity
Is your organization effectively tracking and reporting on APP productivity?
Dive deeper into the latest APP benchmarks on work RVUS, collections, patient visits and more!
As health care organizations look for ways to better utilize and retain their advanced practice providers (APPs), effectively measuring and projecting the clinical productivity of this workforce is imperative. There are several challenges when it comes to tracking individual productivity – especially for those working in inpatient and surgical settings. According to SullivanCotter’s APP Compensation and Productivity Survey, 97% of organizations are able to track individual performance of APPs in the ambulatory setting compared to only 65% in the inpatient setting.
Reliable and consistent productivity metrics are important for organizations to appropriately set work effort expectations and reward high performance.
SullivanCotter’s suite of APP workforce surveys provide insight into APP productivity data and ratios, collections, physician-to-APP staffing ratios, and work expectations. Participating organizations include independent hospitals, health systems, academic medical centers and more.
Press Release | SullivanCotter Opens Participation for 2025 Health Care Compensation Surveys
Support your workforce strategy with industry-leading benchmarks!
JANUARY 22, 2025 – SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and data products for health care and not-for-profits, recently opened participation for its annual suite of health care compensation and workforce productivity surveys.
For more than 30 years, SullivanCotter has provided critical benchmarks and comprehensive total compensation information, analyses, and research to the nation’s top hospitals and health systems. The firm’s market-leading surveys combine data-driven intelligence with national insights to help organizations confidently manage their total rewards strategy across the entire workforce.
SullivanCotter’s longstanding flagship surveys include:
- Health Care Management and Executive Compensation
- Physician Compensation and Productivity
- Advanced Practice Provider Compensation and Productivity
- Health Care Staff Compensation
These are part of a larger and more robust survey suite that also includes insight into registered nurses, benefits practices, physician and medical group executives, on-call pay programs, hospital-based physicians, and more.
“Health care is constantly evolving, and our clients require meaningful data and insights to help navigate unprecedented workforce challenges. Our proprietary surveys enable them to keep pace with an evolving marketplace and develop compensation strategies to attract, engage, and retain top talent,” said Ted Chien, President and CEO, SullivanCotter.
Participants receive substantial discounts on the full survey reports, early access to electronic survey results, invitations to webinars led by our experts, and a dedicated team on hand to assist with questions.
To participate in or learn more about any of SullivanCotter’s surveys, please contact us via email or by phone at 888.739.7039.
Note to media: Data and interviews are available on request.
—
About SullivanCotter
SullivanCotter partners with health care and other not-for-profit organizations to understand what drives performance and improves outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, and data products to help organizations align business strategy and performance objectives–enabling our clients to deliver on their mission, vision, and values.
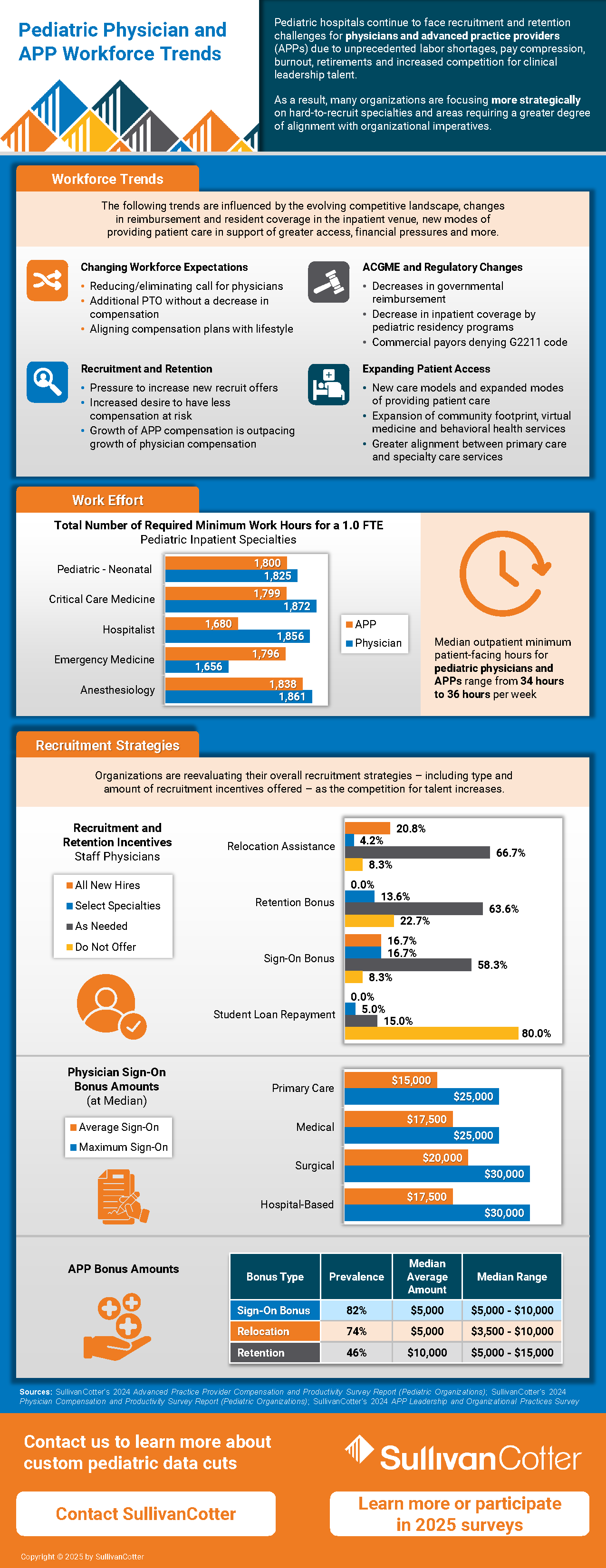
INFOGRAPHIC | Pediatric Organizations: Physician and APP Workforce Trends
Dive deeper into the latest workforce trends and data!
Pediatric hospitals continue to face recruitment and retention challenges for physicians and advanced practice providers (APPs) due to unprecedented labor shortages, pay compression, burnout, retirements and increased competition for clinical leadership talent. As a result, many organizations are focusing more strategically on hard-to-recruit specialties and areas requiring a greater degree of alignment with organizational imperatives.
SullivanCotter highlights some of the emerging workforce trends driving these challenges:
- Evolving workforce expectations
- ACGME and regulatory changes
- Expanding patient access
- Upward pressure on APP compensation
As a result, pediatric hospitals are reevaluating their overall clinical recruitment and retention strategies – including type and amount of incentives offered – as the competition for talent increases.
We’ve compiled the latest benchmarks on work effort and type of and amount of incentives offered to show how organizations are responding!
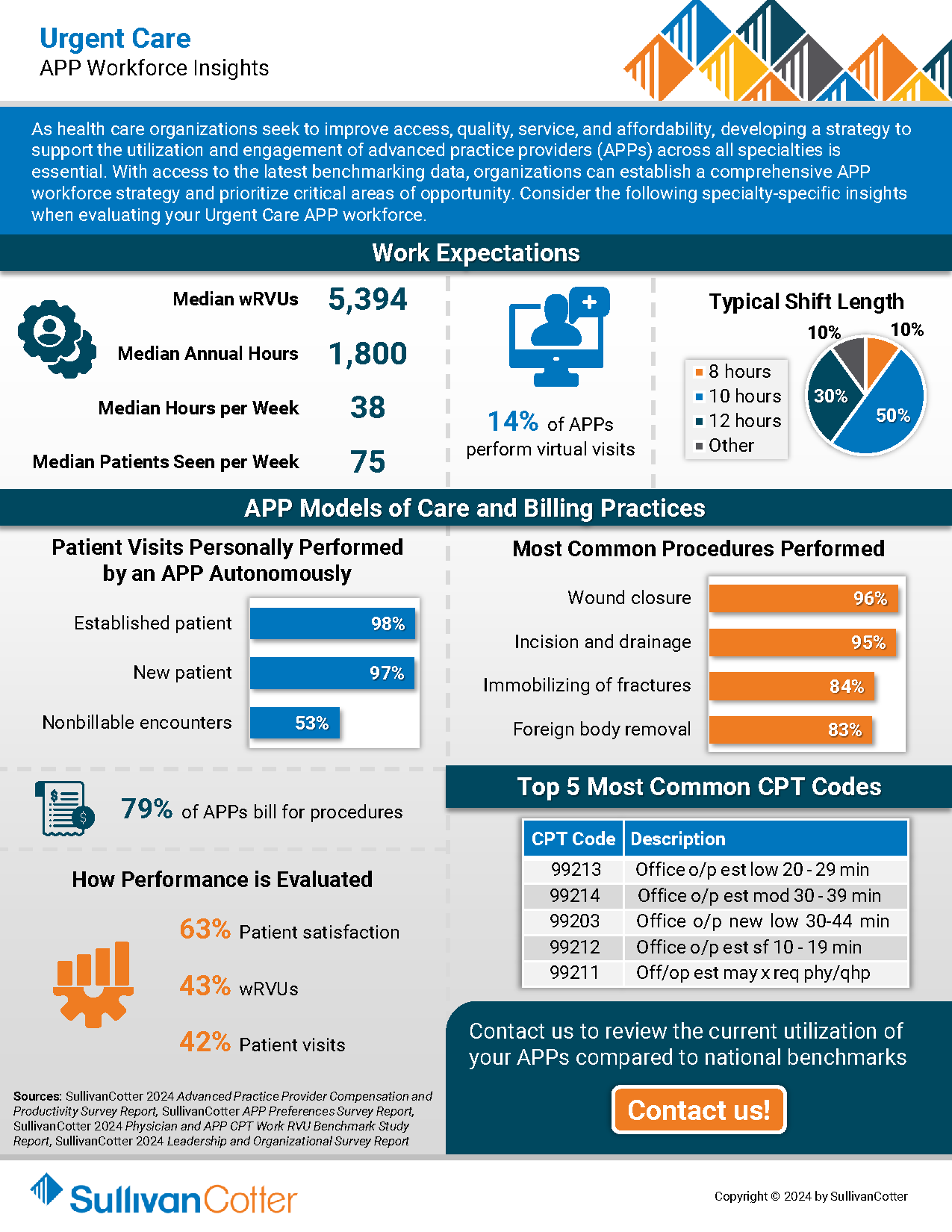
INFOGRAPHIC | APP Workforce Insights: Urgent Care
Learn more about APP work expectations, models of care, billing practices and more within Urgent Care settings.
As health care organizations seek to improve access, quality, service, and affordability, developing a strategy to integrate, optimize and engage the growing advanced practice provider (APP) workforce across all specialties is essential.
Urgent care is an important pathway for patients with more immediate care needs and health concerns. With their ability to provide a more cost-effective alternative to physician visits, enhance patient access, decrease patient wait times and more, the role of APPs within this setting continues to expand.
With the latest optimization and utilization benchmarking data, organizations can establish a comprehensive APP workforce strategy and prioritize critical areas of opportunity. Consider the following specialty-specific insights into Urgent Care setting when evaluating your APP workforce.
Press Release | Median Base Pay for Registered Nurses on Track for 3%-4% Annual Increase to Close Out 2024
As critical staffing issues persist, organizations are looking for better ways to recruit and retain RNs in a competitive talent market.
JANUARY 9, 2025 – SullivanCotter, the nation’s leading independent consulting firm in the assessment and development of total rewards programs, workforce solutions, and data products for health care and not-for-profits, has released the latest benchmarks from both its 2024 Health Care Staff Compensation Survey and 2024 Registered Nursing Compensation Survey.
Collectively, these surveys report data from more than 2,400 organizations on approximately 2.2 million nurses and other clinical and non-clinical employees – representing the largest and most comprehensive health care staff compensation resource for hospitals and health systems.
Health care organizations continue to face unprecedented clinical workforce shortages. The registered nurse (RN) workforce has been hit particularly hard due to post-pandemic burnout, unfavorable working conditions, and an insufficient pipeline of future clinicians. As critical staffing issues persist, organizations are looking for better ways to recruit and retain RNs in a competitive talent market.
Although median base pay for RNs is up nationally by 3.0% according to SullivanCotter’s Health Care Staff Compensation Survey, there are variations between urban, rural, and major metro areas within each region that make it necessary for organizations to dive deeper into the data when evaluating market rates.
Differences in RN Base Pay by Location
With local labor markets being a major factor in many recruitments, it is important to understand the unique nuances of each organization’s geography. Growth in median base hourly rates for RNs is highest in the Northeast (4.8%) and North Central (4.6%) regions, dipping more than a percentage point in the West (3.5%) and Southeast (3.3%). The South Central states showed no year-over-year growth likely due to the 2023 survey results reporting the highest increases of any region.
Drilling down even further into greater metro areas reveals variation as well. When compared to the broader workforce, RN base pay has a higher geographic differential to national rates across six major metro areas. In New York City, base pay is 39% above the national median for RNs and 23% above the national median for all health care staff. This is similar for Boston at 35% and 18%, respectively. These findings indicate that using a single geographic factor for comparing national rates across the workforce in major metro areas is less effective than multiple geographic factors based on job type.
Tracking Changes in 2024
SullivanCotter’s new Registered Nursing Compensation Survey tracks trends in RN compensation on a six-month cadence. Due to external market pressures and evolving workforce trends, many organizations are assessing changes in pay, hot jobs, and movement by specialty more than once per year. The 2024 report, which includes six-month percentage change data from January – July 2024, shows that staff RNs involved in direct patient care have already seen a median increase in base pay of 2.0%. This is slightly less (1.4%) for those in indirect patient care. Both, however, are on track for annual increases of 3%-4% as 2024 comes to a close.
This survey also highlights which specialties have experienced the greatest base pay increases through July 2024. These include Critical Care, Obstetrics, Forensics, Emergency Medicine and Neonatal-Perinatal Medicine.
RN Pay Structures and Experience Pay
This new survey also provides insight into RN base pay by level and experience. Given the increasing prevalence of unionization, understanding the difference between step structures and more traditional pay structures is important to designing an effective compensation program.
Step structures are often leveraged in environments that have an increased presence of unions. Median base pay is higher nationally than in organizations without these structures, and the difference in pay from entry into the field to the final step is greater. The national median for step 1 is $42.49, while the median for less than 3 years of experience is $40.12 per hour. Advancement within a pay range also indicates higher year-over-year annual increases in step structures than traditional structures.
Considerations for 2025 and Beyond
External health care market forces continue to change how organizations are responding both strategically and operationally to recent RN workforce challenges. While pay decisions are nuanced and require a customized approach – especially based on the specific market in which each organization operates – there are several important planning considerations to take into account:
- While understanding national and regional changes in base hourly rates is important, leveraging local market data and pay differentials within major metro areas can assist in making difficult pay decisions and bolstering your competitive strategy.
- Reviewing year-over-year changes may no longer be enough when evaluating the competitiveness of base pay. With RNs often being one of the largest groups on payroll, analyzing market rates every six months will allow for more timely tracking and decision-making – especially for key nursing specialties and setting designations.
- Market movement for RNs continues to outpace that of the broader health care staff workforce. As a result, RNs often require more advanced compensation solutions to carve their workforce out as a priority and help support a more competitive recruitment, retention, and engagement strategy.
- With limited budget availability, evaluating nursing structure components such as clinical reporting relationships, spans of control, and organizational levels may help to improve productivity.
For more information on SullivanCotter’s surveys, please visit our website at http://www.sullivancotter.com/ or contact us via email or by phone at 888.739.7039.
Note to media: Additional data and interviews are available on request.
—
About SullivanCotter
SullivanCotter partners with health care and other not-for-profit organizations to understand what drives performance and improves outcomes through the development and implementation of integrated workforce strategies. Using our time-tested methodologies and industry-leading research and information, we provide data-driven insights, expertise, and data products to help organizations align business strategy and performance objectives–enabling our clients to deliver on their mission, vision, and values.
VIDEO | What is the future landscape of CRNA compensation?
The demand for CRNAs is greater than ever. Compete more effectively for talent with insights from our experts!
Learn more from our ongoing video series.
What is the future landscape of CRNA compensation?
Median total cash compensation for CRNAs has increased more than 20% in the past five years. SullivanCotter’s Sarah Kasner recently sat down to discuss emerging trends in CRNA compensation and how organizations can compete more effectively for talent as demand continues to place upward pressure on pay.
Looking for additional insight?
Dive deeper into the latest benchmarks
Round out your CRNA workforce strategy with insight into compensation, pay practices, work effort, employment status and more!
INFOGRAPHIC | 2024 CRNA Compensation and Pay Practices
CRNAs play a critical role in meeting anesthesia coverage demands.
Is your organization effectively recruiting and retaining these providers?
Gain access to important compensation and pay practices benchmarks!
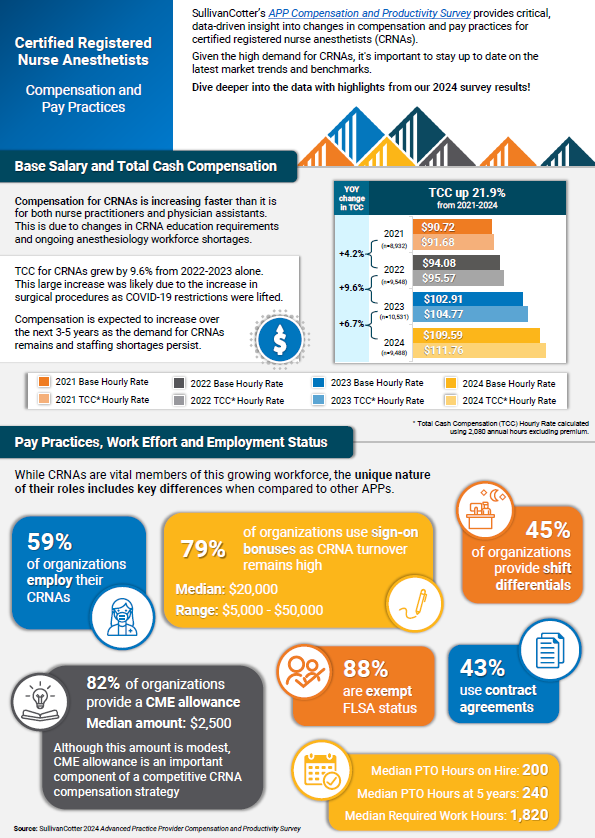
SullivanCotter’s APP Compensation and Productivity Survey provides critical, data-driven insight into changes in compensation and pay practices for certified registered nurse anesthetists (CRNAs). Given the high demand for CRNAs, it’s important to stay up to date on the latest market trends and benchmarks.
Compensation for CRNAs is increasing faster than it is for both nurse practitioners and physician assistants due to ongoing anesthesiology workforce shortages. Total cash compensation for CRNAs grew by 9.6% from 2022-2023 alone. This large increase was likely due to the growth in surgical procedures as COVID-19 restrictions were lifted. It is expected that compensation will continue to increase over the next 3-5 years as the demand for CRNAs remains and staffing shortages persist.
Learn more from the latest results – including insight into base salary, total cash compensation, pay practices, work effort, and employment status!
VIDEO | Considerations for Creating an Advanced Practice Provider Leadership Structure
Leverage the full potential of your growing APP workforce!
Learn more from our ongoing video series that provides insight into emerging workforce trends.
What is the best way to align your APP workforce with system-wide goals?
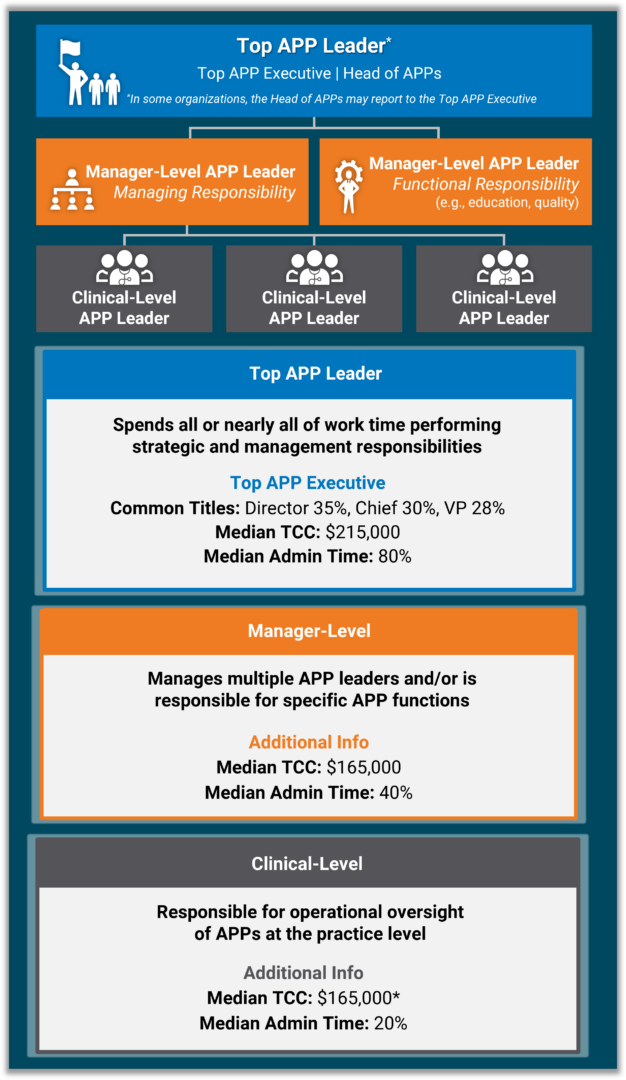
Developing a well-defined APP leadership structure can help to ensure that all APPs are integrated into existing initiatives that focus on quality of care, patient outcomes, and operational efficiency.
SullivanCotter’s Hadley Powless explains how health systems can do this more effectively!
Looking for additional insight?
Dive deeper into our APP leadership data!
Round out your APP workforce strategy with insight into four different leadership levels – including compensation, administrative time, common titles, and more.
CASE STUDY | Maximizing Value-Based Reimbursement
Looking to align compensation more effectively with payer contracts and incentives?
Learn how a large not-for-profit health system partnered with SullivanCotter to improve its value-based reimbursement strategy.
Moving forward in a new value-based environment, health care organizations must align clinical compensation with reimbursement programs to maximize payer contracts and incentives.
However, this approach can be difficult to navigate without the data-driven insights and expertise needed to inform strategic compensation design.
Discover how SullivanCotter helped a client to improve its value-based reimbursement strategy by:
- Creating distinct physician compensation plans by specialty grouping
- Aligning incentives with payer contracts to improve patient outcomes and cost efficiencies
- Ensuring regular reporting through the Clinician Nexus platform
- …and more!
View the case study for greater insight into this organization’s challenges, our approach, and the outcomes!
How Pomona Valley Hospital Medical Center Developed a More Strategic Approach to Physician Recruitment
Leveraging Data-Driven Insights and Expertise to Enhance Physician Recruitment
THE SITUATION
Pomona Valley Hospital Medical Center (PVHMC), a 427-bed not-for-profit community hospital in Southern California, faced the challenge of effectively managing its physician recruitment efforts. As a standalone medical center, it was vital for the hospital to maintain a robust physician network while navigating California laws that prevent direct employment of physicians. The hospital also needed to ensure that its recruitment strategies would be data-driven for validation purposes and compliant with regulatory requirements.
Before partnering with SullivanCotter, the hospital relied on physician-to-population rates published by an external vendor to assess physician supply and demand in its market. Leveraging this data was a manual, labor-intensive process, and the information required greater accuracy and in-depth analysis to make informed decisions and validate recruitment needs. A more efficient approach was necessary.
Accessing the right data and analytical tools would enable the hospital to anticipate community needs and plan, justify, and execute its recruitment initiatives more efficiently. The hospital required a sophisticated solution that could help support this strategy and maintain legal compliance throughout each step of the recruitment process.
THE APPROACH
PVHMC turned to SullivanCotter’s Provider Needs Assessment (PNA), an interactive cloud-based application, to address its recruitment challenges and reach its goals. Several hospital leadership team members, including the Vice President of Administration, the Vice President of Ambulatory Services, and the Executive Director of Planning, collaborated with SullivanCotter’s consultants to implement the PNA.
The PNA provided PVHMC with a comprehensive analysis of physician supply and demand in its service area, including detailed data on the composition and practice patterns of the local physician community. This enabled the hospital to validate the need for specific physician specialties and ensure its recruitment efforts aligned with community health needs.
The hospital’s cross-functional team worked with SullivanCotter’s consultants to customize the PNA data and insights to focus on the hospital’s unique market dynamics and strategic priorities. This collaborative approach allowed PVHMC to leverage the expertise of SullivanCotter while ensuring the information gathered was personalized.
“The PNA lifted a significant burden by giving us more precise, data-driven insights into our physician community and their practice patterns. It became essential in ensuring compliance and strategically justifying the recruitment of key specialties, allowing us to make informed decisions that align with our community’s health needs,” said Leigh Cornell, Vice President of Administration, PVHMC.
OUTCOMES
Implementing the PNA has helped PVHMC improve its operational efficiency and overall recruitment strategy in several ways:
- The hospital now has access to data-driven insights that enable it to make informed recruitment decisions while remaining compliant. The PNA allows for more robust assessments of physician supply and demand, helping to validate recruitment initiatives with the leadership team and board of directors.
- The hospital developed a more strategic approach to physician recruitment. It can identify potential gaps in physician coverage and better engage with community physicians to understand their practice plans and expansion opportunities.
- SullivanCotter’s PNA offers a more in-depth analysis of the local physician market. SullivanCotter’s PNA captures the full complexity of physician supply and demand. The hospital can now identify physicians who only practice part-time in the service area or have satellite offices outside the primary service area. This provides a more accurate picture of physician availability and assists in recruitment.
“If I needed to recruit physicians, I would use the tool to indicate if we have justification and to show our leadership and CEO. We would see the list of physicians in our community and determine who we need to learn more about or see if there’s an opportunity before we recruit to understand and engage with that physician. We can see if there’s an opportunity either for them to expand their practice or for them to come to us, or if there are barriers to such,” Cornell added.
LESSONS LEARNED
The PVHMC case study offers several lessons for organizations considering a PNA:
- Dedicate time and resources: Engaging cross-functional stakeholders and ensuring they understand the data’s implications is essential for maximizing its value. This investment enables more informed decision-making and a stronger alignment with organizational goals.
- Customize the data to fit organizational needs: While the PNA provides a strong foundational framework, working closely with SullivanCotter’s consultants to tailor the data to your specific market dynamics is critical. This customization involves identifying relevant service area ZIP codes, securing accurate affiliation and employer data, and actively working with the information to build confidence.
- Shift to proactive decision-making: PVHMC transitioned from a reactive recruitment strategy to a more proactive one by embedding the PNA into its strategic planning process. This shift enabled the hospital to anticipate and address physician shortages and community health needs more effectively rather than reacting to gaps as they occurred.
- Use data to validate recruitment efforts: The PNA’s detailed analysis offers clear, data-driven justification for recruiting specific physician specialties. This helps secure the support of key stakeholders, such as leadership teams and boards of directors, and ensures alignment between recruitment initiatives and the broader organizational strategy.
INFOGRAPHIC | APP Leadership Structures Can Support Retention and Engagement
Advanced practice providers are integral to effective and efficient health care delivery.
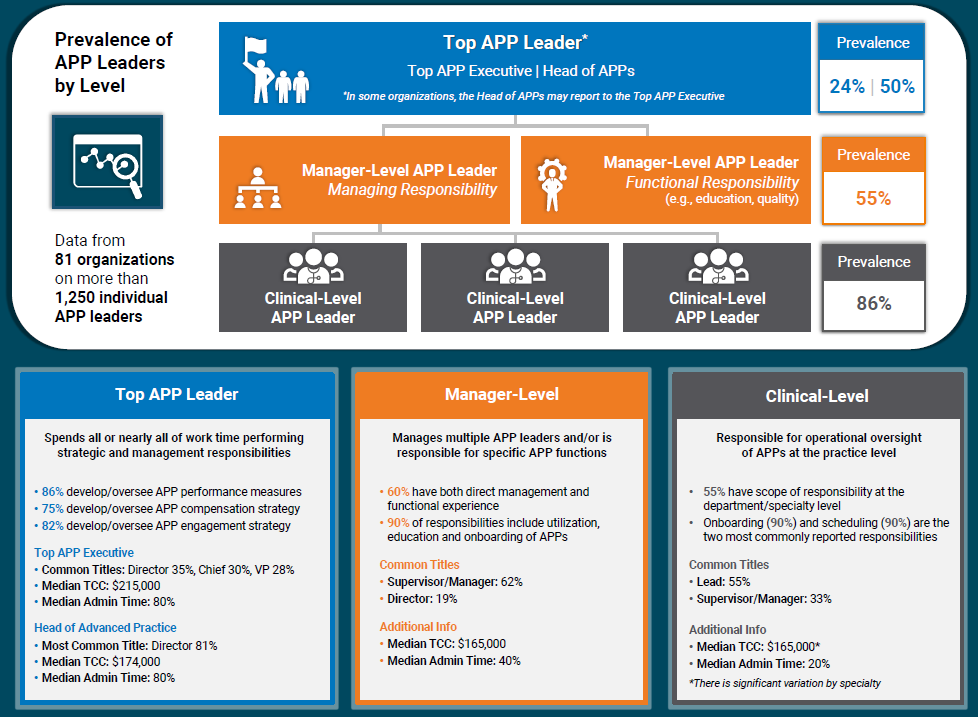
Enhancing your APP leadership structures can help to support APP engagement, workforce planning, recruitment and retention, and greater alignment with physician workforce strategies.
SullivanCotter research shows that the presence of an APP leader is associated with 2% less turnover. With the direct cost of turnover estimated to exceed $120,000 per APP, this can have a significant financial impact on an organization. Additionally, many organizations are looking to have greater consistency in APP leadership leveling, compensation, and administrative time – and require access to the right data in order to address this.
Dive deeper into the data with our latest infographic! SullivanCotter’s APP Leadership and Organizational Survey – which contains data from more than 81 organizations on more than 1,250 individual APP leaders – reports on four different leadership level, including clinical-level, management-level, head of advanced practice, and top APP executive. This includes compensation data, common titles, administrative duties and more.
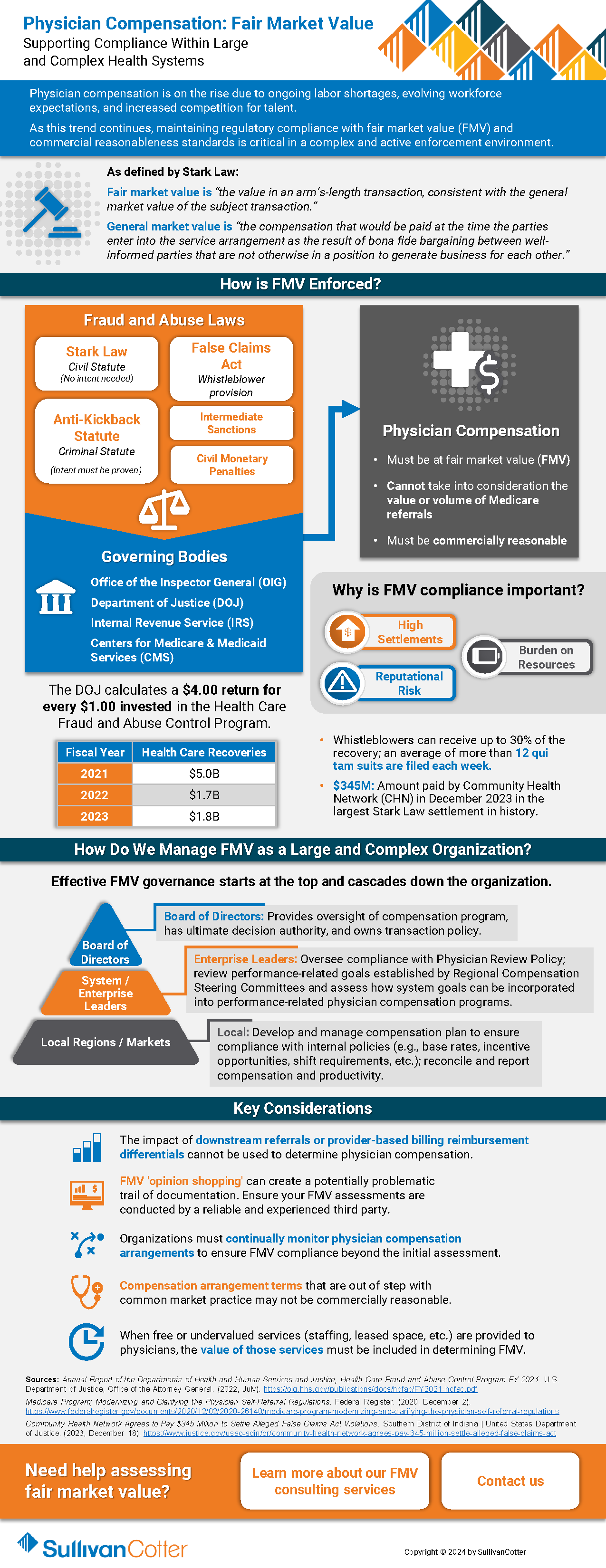
Fair Market Value: Supporting Compliance Within Large and Complex Health Systems
Physician compensation is on the rise due to ongoing labor shortages, evolving workforce expectations, and increased competition for talent.
As this trend continues, maintaining regulatory compliance with fair market value (FMV) and commercial reasonableness standards is critical in a complex and active enforcement environment.
Health care organizations must have the appropriate structures in place to help mitigate financial, resource and reputational risk for potential physician compensation violations related to the Stark Law, the Anti-Kickback Statute and IRS not-for-profit regulations.
Download our latest overview to gain greater insight into the following questions:
- How FMV is enforced?
- Why is FMV compliance important?
- How can we manage FMV as a large and complex health care organization?
- What are some of the key considerations and best practices for supporting compliance?
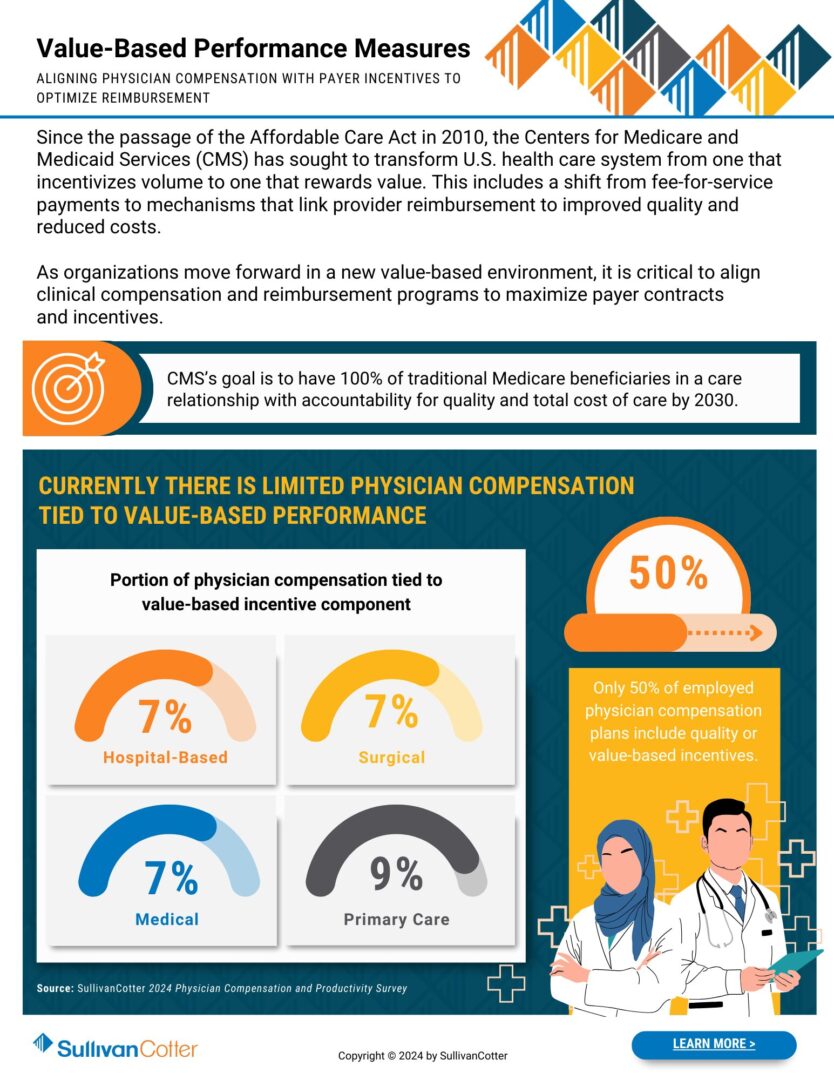
INFOGRAPHIC | Value-Based Performance Measures
Optimize reimbursement by aligning physician compensation more closely with value-based payer incentives.
Since the passage of the Affordable Care Act in 2010, the Centers for Medicare and Medicaid Services (CMS) has sought to transform the U.S. health care system from one that incentivizes volume to one that rewards value. This includes a shift from fee-for-service payments to mechanisms that link provider reimbursement to improved quality and reduced costs.
As organizations move forward in a new value-based environment, it is critical to align clinical compensation and reimbursement programs to maximize payer contracts and incentives.
CMS’s goal is to have 100% of traditional Medicare beneficiaries in a care relationship with accountability for quality and total cost of care by 2030.
Where does your organization stand?
Download our infographic to learn more about incorporating value-based performance measures into your design process.