Utilizing Physician FMV Assessments to Guide Strategic Workforce Decision-Making
It’s more that just a ‘box-checking’ exercise!
Originally published by the American Association of Provider Compensation Professionals
Written by Dave Hesselink – Managing Principal, SullivanCotter and Clara Hurtt – Principal, SullivanCotter
Healthcare continues to grow more complex as organizations respond to ongoing operational, financial, and workforce challenges. To help aid in recruitment and retention, advance key value-based goals, support a variety of physician-hospital affiliation relationships, and often a dynamic combination of several factors – physician compensation is evolving in kind. Moreover, as clinical workforce shortages loom large, the need for competitive compensation arrangements in a tight market for talent is greater now than ever before.
As pay practices change and priorities shift, it’s important to review physician compensation regularly. Most organizations conduct an annual or biannual Fair Market Value (FMV) market assessment to satisfy an internal governance or oversight requirement. The value of conducting an annual FMV review, however, goes well beyond a compliance ‘box-checking’ exercise. Results and observations from these assessments can act as a catalyst to jumpstart strategic workforce conversations, validate investments made in the physician workforce, and ensure an organization is aligned with market-leading practices.
Market Assessment Benefits
Instead of limiting an FMV assessment to compliance purposes only or deciding an assessment is not necessary, organizations should consider several additional benefits:
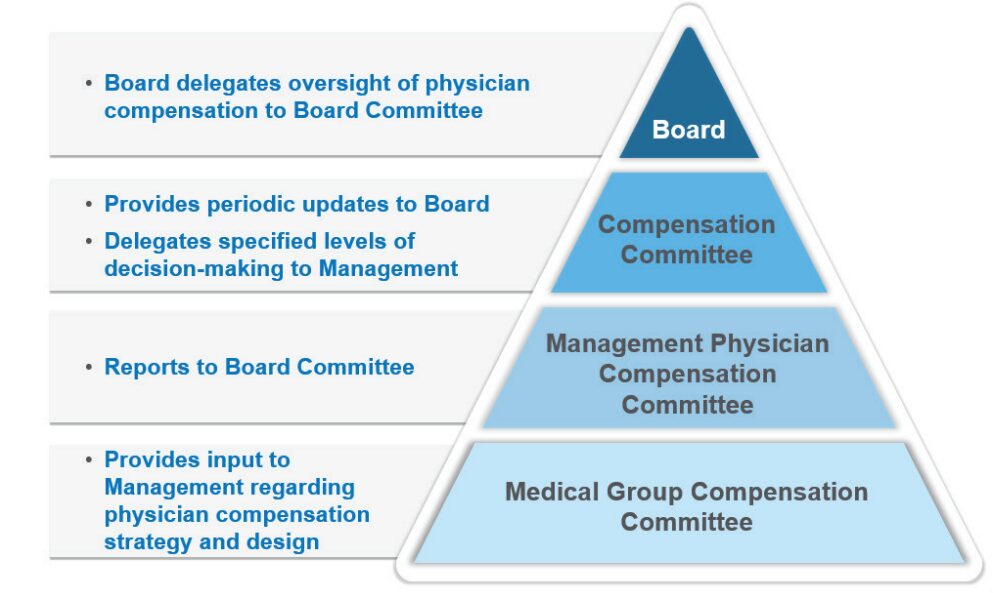
- Opening or enhancing the lines of communication with governance groups: Many organizations have specified Board or Board Committee-level oversight of physician compensation to ensure an understanding of associated compliance risks (see Figure 1 below). With this level of oversight, Boards will better appreciate ongoing recruitment and retention challenges the organization is facing – resulting in a broader discussion of physician compensation from a strategic perspective. This includes physician affiliation and employment and the resulting financial tradeoffs that may be necessary. Board-level engagement in physician compensation is also important from an accountability perspective to ensure management decisions are consistent with an organization’s values and long-term interests. Determine clinician demand, population demographics and payor mix by ZIP code.
FIGURE 1: Typical Physician Compensation Governance Structure
- Illustrating overall market positioning of physician compensation and productivity: Many organizations use regular FMV assessments to track market positioning over time. This serves as a useful gauge of the compensation program’s competitiveness and effectiveness for employed physicians.
- Serving as an important tool for physician workforce planning: A regular FMV assessment identifies physicians who are clinically productive beyond what is sustainable in the long run. These physicians may be highly compensated for their work effort but have a higher potential for burnout – presenting an organizational risk that must be mitigated. It also highlights specialties that are more or less productive than others, pinpoints areas experiencing workforce shortages as indicated by unsustainable productivity levels and helps to determine which specialties may have misaligned work effort expectations – such as an annual clinical work hours expectation that falls short of the market norm.
- Illuminating the effectiveness of the organization’s recruitment programs: Sign-on bonuses, student loan repayment programs, and temporary or long-term housing assistance are all considered economic benefits that must be included when evaluating FMV. The effectiveness of these programs is often reflected by their prevalence and can be evaluated in combination with physician retention rates once these recruitment incentives run their course.
- Identifying outdated compensation rates or pay practices that are no longer necessary: Often these rates or pay practices were adopted to address a particular staffing challenge. For example, the pandemic required extra shift rates to maintain appropriate levels of staffing during an unprecedented industry crisis. Temporary rates were supported from an FMV perspective during this period but are likely not viable long-term. In some cases, unwinding these temporary rates may not have been a priority. An annual FMV assessment can bring these rates to the forefront for review and potential sunsetting.
- Utilizing data collected as part of the FMV assessment to help evaluate pay equity within the physician workforce. Adding ethnicity, gender, and age as required fields within the data collection process can help to flag potential pay inequities. Conducting an effective pay equity assessment requires advanced statistical testing techniques that are not normally included as part of a standard FMV assessment. While an FMV assessment on its own does not satisfy the requirements of a comprehensive and defendable pay equity assessment, it can serve as a catalyst.
The following case study illustrates a practical application of the benefits as outlined above.
Case Study
Health System ABC is a $2.5 billion revenue organization that employs approximately 650 physicians – 65% on an academic track and 35% on a clinical track. Health System ABC conducts an annual retrospective market assessment to satisfy internal compliance and policy requirements. While this annual assessment helps to ensure that compensation aligns with FMV prior to paying year-end incentives, the organization has realized several additional benefits.
1. Determining market competitiveness of compensation
Annual review of aggregate market positioning by specialty highlighted a need to increase pay levels for some specialties to align with the organization’s overall compensation philosophy. In addition, comparing market positioning from year to year demonstrated market movement or more fundamental changes within the workforce.
Figure 2: Comparison of Aggregate Compensation Market Positioning by Specialty
(Current Year versus Prior year)
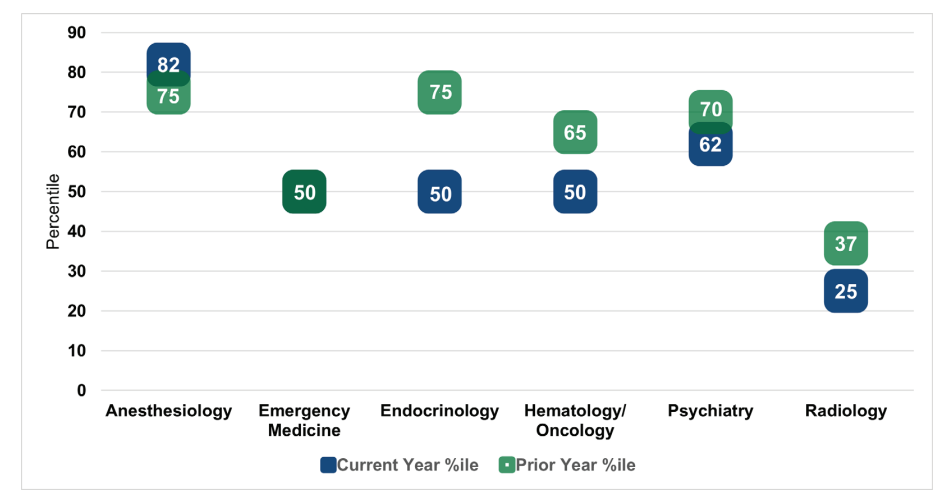
As shown in Figure 2, market positioning for anesthesiology outpaced the prior year by seven percentile points. Upon further research, Health System ABC determined that this finding was a result of short-staffed anesthesiologists picking up extra shifts at premium rates. This validated the need to ramp up the organization’s recruitment strategy for this specialty.
By contrast, current year market positioning for emergency medicine was consistent with the prior year. While Health System ABC had made an important investment into physician compensation within this department, the annual FMV assessment demonstrated that the investment was only just
keeping pace with market movement. Current year positioning for endocrinology, hematology and oncology, psychiatry, and radiology fell below the prior year. After reviewing new hires, terminations, and incentive payouts in each of the specialties, Health System ABC recognized that additional
investments in physician compensation were needed to maintain pace with the market.
Radiology, in particular, fell well below the organization’s target compensation range as defined by the physician compensation philosophy. As a result of their annual FMV assessment and recent recruitment experience, Health System ABC made a strategic decision to invest in this specialty to ward off potential shortages and retention issues.
2. Measuring compensation plan effectiveness
The annual FMV assessment identified several individual physicians whose compensation outpaced productivity. Health System ABC observed that the department distribution methodology for the incentive pool within certain specialties had little to no relation to individual physician performance (e.g., shared equally among the physicians, prorated based on total FTE). This observation provided the organization’s leadership team with a reason to limit the number of distribution methodologies to those that factor in individual physician performance. This made the plan easier to administer and aligned incentives more closely with individual performance and contributions.
3. Eliminating temporary critical staffing rates
Health System ABC’s FMV assessment found that a particular COVID-19 shift coverage rate, which paid hospitalists above the 90th percentile, was still in place 12 to 18 months post-pandemic. While the rate was necessary during the pandemic, it was no longer necessary under current circumstances. After the continued use of this rate was brought to light, Health System ABC worked quickly to assess and eliminate high shift rates. This helped to decrease costs and align rates more closely with the market.
4. Redefining the definition of clinical full-time equivalent (FTE)
As part of the annual FMV assessment, Health System ABC collected data on hours worked in hospital-based specialties. When comparing hours worked for a 1.0 FTE Emergency Medicine physician to the market definition, Health System ABC learned that its FTE requirement was approximately 300 hours less. While the organization couldn’t close the 300-hour gap overnight, this observation led to additional workforce planning discussions with the Department Chair.
5. Aligning leadership rates to the market
Historically, Health System ABC had paid a single hourly rate across all specialties for entry-level leadership roles. By using this approach, the organization was inadvertently disincentivizing physicians in highly paid specialties to accept leadership roles as they could earn more on an equivalent time basis in their clinical roles. With the help of an annual FMV review, Health System ABC implemented specialty-specific leadership rates to more appropriately align leadership pay to the market.
While the ultimate objective of Health System ABC’s annual FMV assessment was to satisfy a compliance obligation, the observations and information obtained throughout the review helped the organization to understand whether workforce decisions and investments continued to align with organizational needs and market-leading practices.
Conclusion
As health care organizations look to design, evaluate, and administer physician compensation in an increasingly complex marketplace, they require a comprehensive governance and oversight process to help support ongoing compliance and mitigate regulatory risk. While many conduct an annual or biannual FMV assessment to satisfy legal obligations, there are additional benefits for organizations to consider as they undertake these evaluations.
These include creating clearer lines of communication with the Board’s Compensation Committee, quantifying market competitiveness, supplementing workforce planning efforts, understanding the effectiveness of recruitment and retention programs, refining or removing outdated pay practices, and providing a baseline for a physician pay equity assessment. Regular FMV reviews are not only an essential component of an organization’s physician compensation strategy, but they can also help to support a more holistic and well-rounded understanding of your physician workforce.